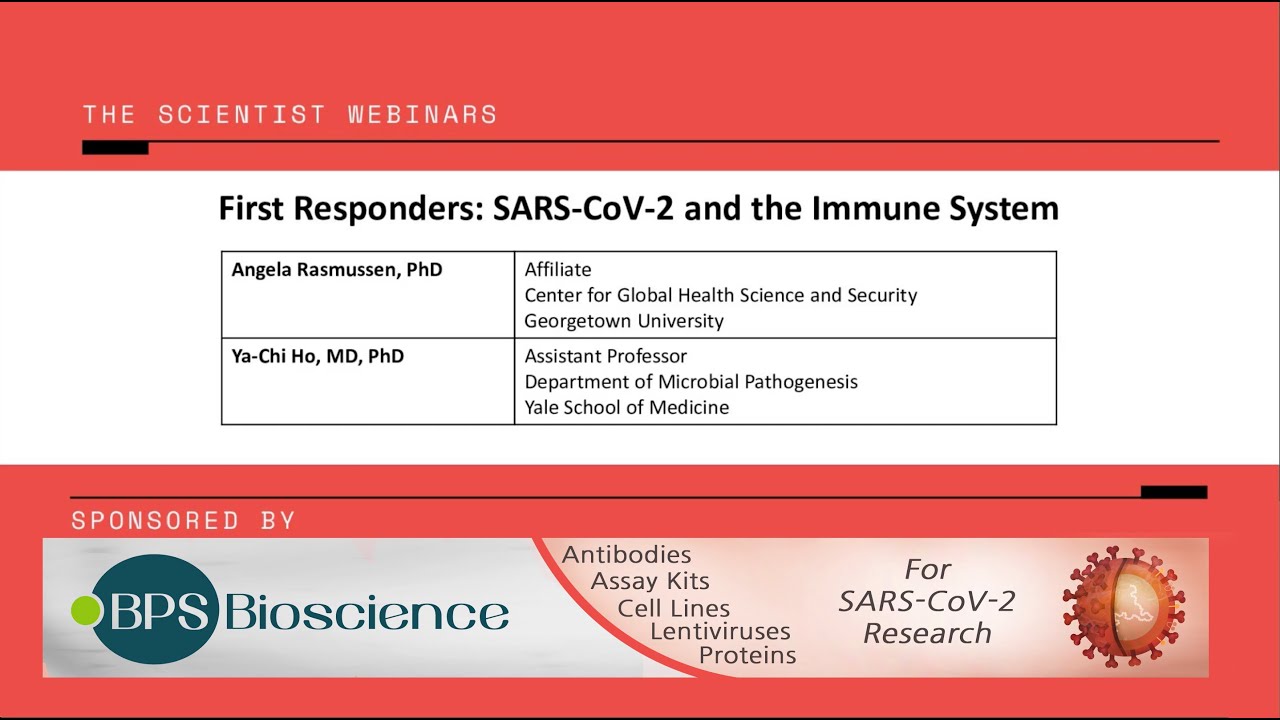
Angela Rasmussen and Ya-Chi Ho explore the positive and negative aspects of the host immune response to SARS-CoV-2 infection and discuss how this knowledge influences therapeutic benefits.
The immune system fights SARS-CoV-2 infection, but it also causes serious clinical symptoms when it rages out of control. In this webinar, Angela Rasmussen and Ya-Chi Ho will discuss how the immune system reacts to SARS-CoV-2, whether these responses are beneficial or deleterious, and the mechanisms by which immune responses determine COVID-19 severity and patient outcomes.
Topics to be covered
– The nature of the host response to SARS-CoV-2
– Understanding adaptive immune responses to SARS-CoV-2 using high-dimensional single-cell profiling
hello everyone and welcome to today’s the scientist webinar my name is nathan knee associate science editor for the scientist and i will be moderating our discussion today our speakers dr angela rasmussen and dr yati ho ho will discuss the positive and negative aspects of the host immune response to tsar’s cov2 infection and discuss how this knowledge influences therapeutic benefits at this time i would like to take an opportunity to thank our webinar sponsor bps bioscience is a us-based original manufacturer with an innovative portfolio of over 4 000 products to assist in your drug discovery projects as a primary manufacturer bps can supply products in large-scale bulk quantities and welcomes inquiries for contract and custom manufacturing within a variety of research areas without further ado let me introduce our first speaker dr angela rasmussen dr rasmussen is a virologist and affiliate at the georgetown center for global health science and security who studies host responses to infection by combining classical virology with modern systems biology approaches her research objectives are to identify host response signatures predictive of infection severity or disease outcome and host pathways to target drug development or repurposing dr rasmussen is particularly interested in viruses that are highly pathogenic and newly emergent or likely to emerge because of climate change land development or ecological disruption dr rasmussen has employed collaborative cross cc mouse models which provide an expanded range of disease presentations to study viral characteristics she developed a cc mouse model of ebola virus disease utilizing the diversity of cc mouse disease phenotypes to study genetic and transcriptomic factors underlying disease severity in humans she is currently evaluating cc mouse models to investigate sex-specific host responses to viral infection as well as disease presentation caused by other viruses that pose a major threat to global public health such as dengue and influenza viruses ultimately these host response profiles can be used for translational or biodefense applications such as diagnosing infection predicting disease severity informing vaccine design and developing or repurposing host targeted drugs to impair virus replication or reverse pathology before we start let’s make sure our your slides are up and running and everything looks good so please take it away dr rasmussen well thank you so much nathan um and uh i’m just going to begin just going to go right into my presentation so before i start all my presentations i like to give a territorial acknowledgement and equity statement and i’m presenting today from seattle uh that’s the unseated ancestral homelands of the duwamish people and much of the work presented today was performed on the lands of the duwamish and the lenape people of manhattan island i acknowledge and honor the first people of these territories as well as their tribal governments their histories and ancestry and their roles today and caring for these lands and i’d also like to acknowledge that there’s a history of systemic inequity in academic science that has spanned for decades and indeed for centuries the institution where much of this work was conducted columbia university was founded using profits from the transatlantic slave trade and excluded women and people of color from the academic community for nearly two centuries this has left a long and painful legacy of racial and gender-based inequality that continues to this day i would encourage all of the folks attending this webinar today to consider how you can contribute to making biomedical and public health research a more equitable enterprise so i’m going to begin by just giving a brief introduction to sars coronavirus 2 which is the virus that causes covid19 um this virus even though it has really profoundly impacted all of our lives around the world um is actually a pretty standard corona beta coronavirus um it is this small particle that has a genome of about 30 uh 30 kilobases it’s a positive sense single stranded non-segmented rna virus that’s in the family coronavirity and it is classified or taxonomically grouped with the beta coronaviruses within its own subgenus the sarbaco viruses or the stars like coronaviruses sars coronavirus ii has unique evolutionary origin and host adaptation and this impacts how it will interact with the immune system of a given host we don’t actually know that much about the origin of this virus but its progenitor viruses likely evolved in bats um it’s unknown whether there was another intermediate species that the virus circulated in before becoming adapted to humans but the virus that is causing the current pandemic is sars coronavirus ii which is um adapted well enough to human hosts it also may be adapting to other new hosts which have the potential to transmit back and forth between the human population anthropologically and zoonotically including cats and mustalids such as minks that have been recently implicated with large outbreaks on mink farms in the netherlands and in denmark and its mechanisms for adaptation because it is a non-segmented virus are through mutation or recombination and this does become important when considering immune responses over the long term uh since this virus can mutate as all rna viruses can that may have implications for uh immunity down the road um so viruses do evolve as they spread through a population and this is the current next strain data showing some of the mutations that have been acquired from different isolates all around the world um and while this virus does have a lower mutation rate than many other rna viruses due to the action of an exonuclease that confers partial proofreading capabilities um this virus is like every other rna virus again evolving as it spreads through the human population and we don’t know that much about specifically what this evolution means in terms of the immune response one of the best characterized variants this so-called d614g mutation in the spike protein has been shown to change the viruses properties a little bit it increases fitness or replication in the upper airway of syrian hamsters which is becoming a leading model for studying covet 19 pathogenesis it also appears to be transmitted more efficiently in hamsters but importantly it doesn’t change sensitivity to neutralizing antibodies um so this is something that is still very much an active area of research trying to understand how this uh how these changes in the viral genome might impact the way that the virus interacts with its host and consequently the implications for immunity or cova-19 pathogenicity um so here’s some host virus interactions that can impact immunity and this is just kind of an overall scheme of the entire immune response and pictured here is influenza virus but um it’s a similar situation for sars coronavirus too in that it infects ciliated cells uh in the airway um but before it even gets there there are passive immune mechanisms intended to keep the virus from infecting cells and that are things like mucus and collectins these are proteins that will just really bind a virus and keep it from doing anything um keep it from getting to the cells that it could actually infect but if you have enough if you’re exposed to a high enough dose of the virus then it probably will encounter uh cells that do express the receptor in this case the molecule ace2 it will enter those cells begin replicating and then a whole bunch of different types of immune responses are triggered initially the innate immune response is mediated both by specialized innate immune cells as well as various pathways within an infected cell um this this type of response is rapid and immediate and it’s also non-specific but i put an asterisk next to that because it’s sort of non-specific some of these cells like nkt cells for example really kind of bridge the innate and adaptive immune system and in addition to that one of the main mechanisms for recognizing viral infection are through so-called pattern recognition receptors or prrs this includes things like the toll-like receptors pictured here as well as the rig i-like receptors which are cytoplasmic pattern recognition receptors and they recognize specific motifs that may not be specific to an individual virus but are generally associated with viral replication such as double-stranded rna so so it is non-specific but it it’s not completely non-specific within one to two weeks the adaptive immune system takes over and this is a very highly specific immune response this is specific for the antigen that that the virus has in terms of its viral proteins uh so this is specific to sars coronavirus 2 and not other coronaviruses or other types of viruses and this involves b cells which produce antibodies as well as t cells which come in two basic flavors there are cd4 helper t cells that coordinate immune responses across the adaptive and innate immune system as well as cd8 positive killer t cells which go out and kill infected cells as is shown here they’re also called cytotoxic t lymphocytes or ctls um this is what we think of uh often when people talk about the immune response they think of antibody titers but the immune system as you can see here is actually much more complicated than that so today i’m mostly going to focus on the innate immune system and how that interacts with the adaptive immune system and the implications for long-term immunity that innate immune responses contribute to so this is an overall uh diagram that’s very simplified but it shows the interferon system and interferon is a cytokine that was so named because it was observed that it interfered with viral replication uh so type 1 interferons in particular are really critical molecules for the innate antiviral response when a virus gets into a cell it comes into contact with one of these pattern recognition receptors in this case uh tlr3 or tlr-789 are pictured here they are are linked to endosomes which are compartments the viruses are internalized in in addition to that there is rig i and mda5 which are in the cytoplasm and once the virus has completed fusion and put its genome into the cytoplasm and begins replicating these can recognize double-stranded rna motifs that are associated with viral genome replication um both of these pathways end up turning on interferon signaling they result in the production of interferon which then is secreted from the cell binds its receptor on another cell and activates this jack stat signaling pathway which then results in the expression of so-called interferon stimulated genes or isgs and i included uh this separate um picture of these spartan soldiers here as the isgs because isgs come in a variety of different flavors and functions um they do all sorts of different things from directly attacking viruses or viral proteins or viral replication products um to turning off or modulating the host to deter or suppress viral replication so there’s a lot of different specialized isgs that have different functions but all all of these processes are really critical to mounting an effective antiviral response particularly early in the infection so viruses have evolved over time all these different mechanisms for blocking this system viruses can block pattern recognition by interfering with these pattern recognition receptors ability to recognize virus motifs they can silence signal transductions so they can dephosphorylate some of these signaling molecules prevent them from basically getting into the nucleus and starting to express interferon itself they can shut down interferon production or block its secretion from an infected cell in addition to that in the cell that would be the target of that interferon signaling they can block the jack stat signaling pathway by a variety of different mechanisms one of which is blocking stat dimerization so stop activated stat molecules have to form these dimers before they can enter the nucleus and act as transcriptional activators um it can block nuclear translocation and it can also prevent isg expression and some viruses have also evolved the ability to inhibit specific isgs that are important uh for counteracting those specific types of viruses so the the virus and the the host interactions and the immune response is really a very complicated dance in which uh either partner is constantly trying to step on the other partner’s toes or mess up their steps um and it’s you know an ongoing struggle uh throughout evolutionary history that’s a really fascinating um area of study from my personal opinion so how does this um impact sars coronavirus 2 and kovid well some work out of ben tenover’s lab at mount sinai shows that sars coronavirus 2 infection in ferrets and in cells as well as in human patients really profoundly suppresses both type 1 and type 3 interferon responses and type 3 interferon responses are also thought to be important for innate antiviral function um they do that more profoundly than other common respiratory viruses such as seasonal influenza virus and one consequence of this is that in shutting down these interferon pathways they’re actually also shutting down uh regulation of many of the other inflammatory pathways that uh talk a lot there’s a lot of crosstalk and redundancy between many of these anti-viral signaling pathways and that does include signaling for a number of different pro-inflammatory pathways so the consequence of shutting down type 1 interferon is not just that the virus can grow better but also that it up regulates the expression of all these inflammatory cytokines and chemokines that then recruit inflammatory cells to the site of infection in the lungs and this has been proposed as a mechanism uh for which uh covid19 actually occur outside of stars coronavirus 2 infection so sars chronovirus 2 infection is shown by the same group does induce very unique host responses that are very different from the types of responses that are induced either by influenza a virus and influenza a virus that is unable to antagonize interferon or treatment with interferon itself um the the gene expression profiles of cells infected with stars coronavirus ii are very different as shown here on this principal component analysis when you look at the pathways that are induced like what do these genes actually do biologically you can see that they also have very um significant differences in terms of the genes that are classified as being involved in interferon signaling or response to viruses response to cytokines and regulation of map kinases which is an important pathway for inflammation so it really does look like sars2 is able to manipulate the host response in a way that that is probably favorable to its replication and as i mentioned just a moment ago the effect of innate immunity on inflammation is really important in terms of the pathogenesis of covid19 so forgive me this diagram is a little confusing but what goes on here this is basically showing two different scenarios it’s showing the virus infecting a cell and the effects that it has on that cell directly and then it’s also showing some of the responses that happen so all these inflammatory cytokines and chemokines start getting secreted there’s all this communication and positive feedback with both cells of the adaptive immune system as well as cells of the innate immune system such as monocytes and macrophages then it can go one of two ways you can have a healthy immune response in which inflammation is controlled effectively antibodies are produced t cells are produced and begin infect eliminating infected cells um virus release is stopped replication is stopped and the infection is cleared there’s this other situation however where there’s a dysfunctional immune response in which all these pro-inflammatory cytokines begins being secreted people are calling that the cytokine storm it basically means uncontrolled expression of pro-inflammatory cytokines this can have a pretty profound impact on the function of t cells and b cells down the road so it is thought that an aberrant immune response to infection really leads to severe coven 19 and that’s what i’m going to talk about a little bit more today so we don’t really know much about the mechanism by which sars coronavirus 2 can antagonize the interferon system but one group has actually started to look at this fairly systematically and they’ve identified a variety of different viral proteins that have an effect on uh on these pathways that i just told you about so they can both impact this in terms of shutting down signal transduction from the pattern recognition receptors in this case they’re showing rig eye and that prevents interferon from being expressed at all in cells that are not infected or sorry cells that are infected but have not yet had interferon be activated they can also um impair stat signaling so this is uh involved in signaling and expression of those isgs that i mentioned so they can block that in a couple of different ways both by blocking the formation of stat 1 and 2 activated dimers as well as blocking the ability of that those activated stat 1 and 2 complexes from entering the nucleus and beginning to express isgs um so we wanted to know my group wanted to know and i’m just going to show you a little bit of primary data um how this worked systemically because we know from ben 10over’s work that sars2 can suppress interferon but what is the what is the consequence in a model of actual cova 19 disease so we use the rhesus macaque model um collected whole blood samples from infected rhesus macaques over a 21 21-day time course and then we performed rna-seq to identify systemic host response signatures in the peripheral blood and it’s important to note that the rhesus macaque model is a model of moderate covid19 these animals do have pathological evidence of disease as well as evidence of pneumonia and infiltration on x-ray uh however they they don’t really get that sick and they recover so this is not a model of really severe cova-19 um but it is a tractable animal model to study this in so what we saw when we looked at our data was actually very different from what the 10 over lab saw in infected lungs and it’s important to note also that in the peripheral blood in these animals there was absolutely no virus so we’re looking at cells that are not infected um against systemic responses and we saw that that interferon all of these pathways related to those innate antiviral responses that i just told you about are actually really upregulated um early on in infection suggesting that while it may be suppressed in the lungs the cells that are actually being infected systemically there is an effective immune response and we also saw looking at the cellular level this is a method of using transcriptomic data to infer which kind of immune cells are driving those signatures we saw that there was an increase in relative myeloid and phagocytic cells so these cells that are involved in the innate immune response and are really important in controlling inflammation so antigen presenting cells that go on to activate t cells um as well as macrophages uh that are really important inflammatory effectors those are increased in the peripheral blood which makes sense with what we know in the context of an acute infection these cells are being mobilized from the periphery to go into the lung and begin clearing the virus infection we also see an increase in plasma cyto dendritic cells which are highly specialized secrete type 1 interferons suggesting that they are mounting effective systemic interferon responses and in this model um as i mentioned this is moderate covet 19 but these systemic innate immune responses appear to be intact even if they’re not in the cells that are directly infected this seems to be supported by some data that that came out of the clinic in which decreased interferon and isgs were observed only in the peripheral blood of patients who had severe or critical cova 19 but not in cases of mild or moderate coca-19 which is consistent with what we see in the rhesus macaque model so um our that led to us developing a hypothesis that we’re trying to test now um that while direct infection may suppress interferon and result in this increased inflammation um leading to this cascade of of apparent immune responses and including aberrant adaptive immune responses in mild to moderate disease um if it’s controlled in the periphery if you have these early interferon responses you can control inflammation so that it’s only directed at clearing the virus but not causing the harmful cytokine storms that are associated with severe disease in severe cases it’s likely that these systemic responses would also be suppressed leading to that uncontrolled inflammation but as i mentioned we still need to do a lot of work to test this hypothesis um and i’m just going to conclude here with some implications for adaptive immunity so as i mentioned um with stars coronavirus 2 infection the innate immune response comes up first that results in the activation of a number of different kinds of cells but especially dendritic cells which are really important in activating t cells and initiating these adaptive immune responses that leads to cytokine production that regulates t cell polarization for example in th1 polarization is thought to be really important for mounting effective antiviral responses in the adaptive immune system also induces a class of t cells that are important for regulating inflammation um as well as t follicular helper cells that are involved in mediating antibody responses and also immunological memory and this is you may have heard that some patients do have declining levels of antibodies in the the months shortly after they’ve recovered from covid and many people have pointed to this as um as waning immunity but i don’t think that’s really a correct interpretation of it i think that it’s it’s very normal for high levels of igg and neutralizing antibody to be produced right during the end of and directly after an acute viral infection but then those antibody levels normally drop down uh and to a baseline level and sometimes they can be undetectable but that doesn’t mean you don’t have immune memory however we have also observed that there are some cases of re-infection and while it’s very unclear whether those people lost immune protection or never had it to begin with it does suggest that in some people anyways they may not be developing as robust of an immune memory response and that was really bolstered by this study that that looked at germinal centers or places basically where where helper t cells t follicular helper t cells are activating b cells to produce antibodies to make those antibodies better and inducing immunological memory in patients who had died of covin19 they didn’t have observable germinal centers in their spleens or lymph nodes where these normally form and they were also associated with these uh cells that were macrophages that were secreting a lot of tnf alpha which is a really potent pro-inflammatory cytokine so that may have actually led to a block in t cell differentiation leading to a loss of immune memory and i think of this as somewhat of a snowball effect um loss of immune memory is a critical problem especially if we’re talking about you know how well protected are people who’ve had coven 19 but you could trace that all the way back to their failure to mount a functional innate antiviral response in terms of interferon expression so this is something again that does require a lot more investigation but i think it’s a really interesting topic and i hope that this segues nicely into dr ho’s presentation which i think is going to focus more on the adaptive immune system so i’m just going to end there by acknowledging the collaborators who contributed to that that work that i showed you from my lab and i’m happy to take any questions during the q a session thank you thank you dr rasmussen for that wonderful presentation as a reminder to our audience you may ask questions at any time using the q a tab our panel will have a chance to address these after our next speaker our next speaker is dr yatchi ho chi ho is an infectious disease physician at the yale school of medicine who studies virus induced immune dysfunction at the single cell level she combines virology molecular biology immunology and single cell rna sequencing to study hiv host interactions in cd4 positive t cells her ultimate goal is to identify mechanisms of hiv persistence and to develop hiv cure strategies dr ho received her md in 2002 and did her internal medicine residency from 2002 to 2005 and infectious disease training from 2005 to 2007 at national taiwan university hospital she became interested in virology research after taking care of hiv infected individuals and sars kovi 1 infected patients in 2003 after one year of practice as an infectious disease attending physician in taiwan dr ho focused on research she received her phd at johns hopkins university in 2013 and continued on her post-doctoral work with robert f siciliano dr ho started her lab at yale university school of medicine in 2017 as an assistant professor in microbial pathogenesis and medicine she is a yale top scholar gilead hiv research scholar and an investigator in the aids clinical trial group so let’s make sure your slides are up and running and everything looks good so please take it away dr ho thank you for having me and thank you so much angela for such a wonderful talk and you really learned a lot from that i’m an hiv researcher using single cell methods to study the rare and heterogeneous population of faith reservoir and hiv-induced immune dysfunction so today i’m going to talk about how single cell methods that we learned from studying hiv can provide detailed and powerful immune profiling in copen 19 and focusing on the role of significant t helper cells in kobe 19. so why is copenhagen different from other viral respiratory infections we actually have learned a lot in sars kobe 1 from researchers such as sting perlman and ralph barry and many others so for example in search code b1 in the animal model uh developed by stately permanent on the left they’ve been showing that well there is already an interferon dysregulation that’s being shown in this animal model so early studies show that uh typically during viral infections such as influenza influenza the inferior should kick in and stop the replication of the virus as angela just talked about however in this model they show that because um starts at both copy 1 and copy 2 now we know they have ways to block interferon responses then this interference response kicking a little bit too little and too late because the timing is too late so the bridge between innate and adaptive immunity becomes messed up so then instead of clearing this viral infection then we see a lot of like cytokine storms that dysregulated adaptive immunity anxiety’s kobe 1. the second difference is that unlike the common code coronaviruses that only colonize the upper airways and unlike starch kobe 2 so sorry the cyroscopy one that’s infecting the lung but not much in upper weary so that it’s spreading it’s not as efficient surge cov2 is both efficient in spreading because it’s in the upper airway in the nose and it’s also like damaging the lung terribly so we have a lot of transmission a lot of mortality and that is different from the previous stars kobe 1. so we want to understand cd4 t cells because we want to control inflammation and disease severity very frequently when patients visit the hospital the presented say with them cough and some kind of fever or dyspnea they’re usually after five to seven days of real the real viral infection or even longer like you know after five seven days of symptoms they visit the hospital but if you think about it at this time when they visit the hospital their viral load already peaked that that it’s already that this regulated interference response is cytokine storms that is kicking in so at this time it may be too late for them to receive an antiviral therapy it’s just too late so to help these people and reduce disease severity we need to understand what happened in this information because many patients when they presented to the hospital that what we’re fighting against is inflammation and it’s already too late to stop right viral replication at that time you can still use antivirals but a lot of things are damaged are done by inflammation and second thing is that we want to understand how to build long lasting and protective immunity and this is review by stim perlman what is shown is that we don’t develop much the cold chemical kernel virus antibodies they just weighing and you get a repeat infection it’s shown in previous nature met people in september but surge one at least we know seems that there is some kind of long-lasting unity that can be detected up to say eleven or seven years in the follow-up we still don’t know about what happening stars could be true and we we’re trying to understand this so why do we care about c4t cells i would like to remind the audience that there is another webinar that’s freely online available talking about b cell responses and antibody durability that is discussed separately that if you’re interested in that we can you can feel free to go to that webinar link but today we’re going to focus on cd4 t cells we care about c4 t cells because they’re the central orchestrator of adaptive immunity so basically cd4t cells have three jobs one it induces robust cda t cell responses so it’s a cd4 t cell help for a cd8 t cell so cdat cells are the main effector the main army to kill infected cells so it needs cd4 help to to induce this robust response and second cd4 t cells themselves can kill infected cells through direct cytotoxicity or through effector cytokines such as interferon alpha interval gamma and tnf alpha so they can have a direct killing especially in cd4 t cells they’re a small subset of them they’re antigen specific c for t cells for example in the case of sars that these are the cells that respond to surge integer stimulation and they will become the memory that later when we get to exposed to this virus again it’s these antigen specific c for t cells that will maintain the memory response the third job that c4 t cells do is that these are specialty follicular helper cells that they live in the germinal centers and they help b cells so basically b cells make the first version of antibody they don’t really work very well but with the help from t follicular helper cells they’re going to go through several rounds of affinity maturation and class switching so that makes good potent and neutralizing antibodies so we think c4 t cells are very important in many viral infections including hiv and copen19 and the second observation is that why is cd4 important is a very early and early as like january people already noticed that in severe cova 19 patients that cd4 t cell count are severe are like largely depleted this is about 200 per per microliter it’s like we almost call this as aids if it’s an untreated hiv infection but this is not aids but we do see like a c4 like low silver count in severe patients across multiple studies and not just that their count is slow but it seems like they may have some impaired function such as interference gamma expression so we want to understand what is wrong and the third thing is that we learned from previous lessons in science code v1 back then in stars kobe 1 that this is a referric study that you know we want to develop search kobe 1 vaccine the easiest way to do it is to take the virus and inactivate them add an aluminum adjuvant injecting to mice this is how say influenza vaccine is given so it is great that it does induce a robust antibody tighter and good response however something went wrong that if you just use this a very typical traditional way to build a vaccine somehow it induces th2 cytokines such as l5 and io 13. so instead of the viral viral killing th1 cytokines it’s toward stage two phenotypes and what is even worse is that it brings a whole lot of eosinophils to the lungs so then mice like older mice in this experiment who got the vaccine and when you challenge them with a real infection they actually perform worse because their lungs are stuck with these eosinophils and they have worse outcome worse mortality so basically that’s the vaccine just just just getting worse so we should replicate this without knowing why but this is showing the importance of whether we can make a vaccine to direct or teach when responses and how do we avoid these side effects so but later on we know this is because of aluminum adjuvant but we just need to understand that t cd4 t cells are also important in vaccine development so why do we see a lot of papers having a single cell high dimensional profiling a whole lot of those and is that just because they are new technologies they’re just fancy so turn out cd4 t cells or immune cells are not really just one single cell like one one single type of cd4s so just cd4s they can have different polarization function and cytokine profiles exhaustion activation memory phenotype energy specificity many different things so taking a recap example um that if we look at all the cells all together it’s trying to guess out what this glass of smoothie has make us have many different kinds of fruit we just don’t understand how many food and which component that is but if we look at them at a single cell level then you can see the proportion of each fruit you can name them you can call them and you can look at the different for example functions or transcription in individual cells so this help us to understand the rare heterogeneous and unknown populations of immune cells and that’s why we commonly see single cell technologies in these copenhagen papers so in the very beginning we’re trying to keep updated on the this current research and with many great great great papers and from many like outstanding researchers around the world and those are just very helpful and informative but the problem is that we notice that there’s not only outbreak of virus there’s also an outbreak of papers it’s just quite hard to keep up with them that that when we write this commonly like like four language papers in two days for example it’s just very hard to chase after them so we’re just sharing how we look at these papers when they come out so we notice that first disease severity matters that whenever we look at a paper is it done in in you know mild cases or in like post-mortem analysis it’s mild or severe and second the timing of the collection of the sample is important for example if the samples are collected right at symptom onset we can capitulate something viral replication going on but whenever the blood is taking during icu admission usually it means that there’s a lot of inflammation going on and there are samples taken like during convalescence the convolutions plasma or during recovery phase after they’re discharged they may have robust c for t-cell responses but they may not re capitulate what’s ramping up in the very beginning and of course asian sex matters so we just look at these different points when we like navigate through the literature so where’s the battlefield of course the lung is the battlefield of kobe 19 because like raspberry failure is the major uh major reason that this is causing death but to study lung is not very easy because these patients already have a very fragile lung you cannot just take a biopsy pocahonta and the patient may just die because of this too invasive procedure so the researchers would take bronco evil watch fluid basically you just um throw some saline in and wash them out and look at what’s the solar component in these and then yeah so their single cell landscape analysis of these immune cells in the lung they found that so the key question is who is making the cytokines and who is causing the cytokine storm there’s been argument like who’s doing it it seems like in this paper it’s shown that it’s the macrophages in the lung they’re making io60 and f and a whole lot of like other like chemokines so then it’s the long macrophages that is initially making all these cytokines that is likely contributing to the overall systemic inflammation or recycling storm they do find expanded clones of cytotype t lymphocytes such as cdt cells in them but it seems it seems like they are responding to this infection secondarily for example in moderate patients they have increased uh t-cell clones or proliferation but in severe cases this proliferation is gone suggesting that the t cells want to come and contribute and control the infection of proliferate but in severe cases these t cells are probably not sufficiently proliferating to to maintain them another study showed that well they look into a different lungs lavage samples across different disease severity so what they found is that these are the cytokine profiles from mild to well moderate to like the severe disease and you can see that these bubbles are looking like bigger and brighter and more this is because the cytokine profile seems to be more like in those people with severe disease so what this paper found is that it’s the infected lung epithelial cells you know they have in a sensing they sends out there’s a virus coming on they started to scream out like cytokines then they recruit non-resident macrophages which means that they secrete these chemokines and macrophages in response to these cause like flush like into into the lung but supposedly this should contain the infection they’re coming to help but because of the cytokine dysregulation these macrophages come and sit there and secrete a whole lot of chemokinesis making extra dates so then the lungs should be like a thin layer of balloon having lots of air exchanging but with all these immune cells squeezing too long with extra days and fluid that people feel like i just cannot breathe because my little balloon is not like a water balloon you cannot breathe and that’s called respiratory failure but this is showing that non-resident macrophages is a culprit producing cytokine storm so what can we do so this recent paper published this week showed that there are ways to intervene into this cytokine storm for example in this mouse model they use tnf alpha interferon gamma antibodies to block hopefully this cytokine storm in the very beginning so then block the downstream signaling that angela just talked about and they show that this can decrease motility and decrease tissue damage whether this can be used in humans is still unknown but it’s a proof of concept mechanistic analysis of what we know about what’s being dysregulated and how we can propose a treatment or immunotherapy the second battlefield is to avoid tissue you’re like why so lymphoid tissue is the home of lymphocytes and also it is the home of b like both t cells and b cells and this is where b cells um getting their education and make high affinity antibodies on the left this is a normal lymph node you see these like bubbles these are the germinal centers or follicles so basically there are t cells and b cells like interacting in there so then b cells make antibody and go to t follicular helper cells and then t follicular helper cells will help class switching and help affinity maturation into the end it makes a good important in neutralizing antibodies but um this is the same study that angela like talked about before that ink disease patients when they look at their lymph node it’s just all wrong so on the left it’s like a typical elementary school you have the structure of a school you have teacher called t follicular helpers and you have b cells called students but in covalent 19 cases it’s all messed up that the structure is not there and and like so this means that there’s no way that b cells can can go through these guided maturity of like of any maturation so to make better and better like anybody’s it’s just o wrong like the the structure is not there and the t cell is lost so this paper concluded that because the loss of t cell follicles and may be a reason why some patients may not develop durable humeral immune responses in copenhagen so if you don’t have t cells you may have problems with your antibody production and finally is the blood so we take blood because you can you can it’s less invasive you can follow patients longitudinally and you can you can look at the immune system using this window we don’t mean that blood like immune profiling is the same as lung because the cells do different things at different sites but this is a window for us to understand the immune system and especially in the blood we’re going to talk about two things so first is cd4 t cells generally overall the other is the antigen specific like such kobe two specific c for t cells that is the one that’s going to develop memory so what happened to them there are typical ways to look at c for t cells in a single cell level so one is using a protein based method such as flow cytometry or mass cytometry so this is a cytoplast or this is backspace so basically you have a selection of antibodies say from 40 to up to 200 if you do sight seek for example that you have the antibodies you know no proteins known proteins that you want to look at can stain them and look at them and second is rna-seq based method that you use rna-seq so it’s a unbiased genome-wise profiling of the transcriptome of individual cells the good thing is that you don’t need to pick what’s already known you just let the data tell you what’s up and down the bad thing is that rna transcription doesn’t really reflect a protein expression so there if you join them together plus clinical uh information plus a viral load plus uh like plasma interference cytokine levels that integrating all these immune data all together then will reach so-called high-dimensional immune profiling for example this one is john query and michael study looking at deep immune profiling of copay 19 patients then combining all these data you know high dimensional flow cytometry of like immune cell markers and then with clinical data and cytokine levels they found that this kubernetes response is it’s just very complicated there are different people who may respond differently they may not be like a one shoes fitting all any response but for example there there is something that’s going to come for example some group of people having a highly activated cd4 and cdt cells that’s also seen in other studies this is akiko iwasaki’s analysis looking at covet knighting patients from very mild to very severe across different time points so this is a yellow impact study a prospectively archived uh like like planet archive a longitudinal study to look at immune profiling over time so what she found is that yeah this is reminding us the th2 dysresculation in the kobe 1 vaccine study remember that we say that in that vaccine study isle 5 and il13 was upregulated and same as here that a kiko’s group found that there is an upregulation and misfiring of teach two phenotype of il5 and il13 that sars infection should should induce type 1 th1 to to fight again get against the virus but there is this th2 misfiring we still don’t know why but this is interesting and second is that there is an upregulation of interferon alpha interferon gamma like the real alpha it’s a little bit too late similar to what we’re learning cytoskeleton it’s there but severe patient you see this peeking up a little bit late the moderate patient it’s like coming down like early so this interferon level is correlating with viral load in the nose and then is correlating with the severity that the more severe you have a stronger and higher level of interference response then using other ways to look at this for example if you look at this another study using systemic biology there are several like different like massimetrine sites seeking different studies all combined in this study you can see that in icu admitted patients in this blue diet it seems like they’re they’re interfering on peaking a little bit late and those moderate patients in the purple dots they’re somewhat peaking early well we’re not sure but this is somewhat similar to who akiko’s group has found what this paper found is that interference response is a little bit too it’s too little and transient it seems to be not enough but what is found is that if you look at the plasma level of interferon is a chlorine floating in the blood this can affect the transcriptome of cells that the receptor kind of blood is affecting the transfusion cells in the blood so it’s correlating with each other so your immune dysregulation in the blood is affecting the immune cells and in their behavior so what this group found was that cd4 t cells have increased expression of inflammation related genes and like they’re just more activated and they have these like phosgene dust and these are likely the things that they propose to cause like this regulation of cd4 t cells and they have lower anti-inflammatory genes in co-19 patients this is a study done by yale showing that there is a dissynchrony between the enemy and death immune system that it’s just regulated because the the sequence of bridge is just sort of broken so finally here’s one question that we asked in the very beginning so why do covet 19 patients have low cd4 t cell count like hiv infects cd4s but starts don’t certain various infections doesn’t infect like c4 t cells so why did they die and where do they go so by single cell earnings seek they found that by comparing corbin 19 and influenza infection oh they found that there is a signature that is different in corbin 19. you see these like il-10 il-6 tnf interferon that these things are going wrong and then when they compared and then copenhagen in control of the donors they found oh it is tnf like trash caspase fast that is up sorry it’s these ones that are upregulated so that it is contributing to the death of cd4 t cells so that’s why they may have a lower c for t sub count so the last study i’m going to talk about in the box c4 level is that this study found is that if you look at viral load in the blood interferon alpha level in the blood and cd4 t cells you can sort of figure out one story that because stars interfere with interferon signaling you have lower levels of interference alpha in critical patients because of that then your source infection cannot be controlled so you have higher level of sars viremia systemically in these patients then because in immunity cannot control this viral infection you’re going to call for the help for for adaptive immunity but this is just too much overwhelming activation so you see activated c4t cells expressing exhaust exhaustion phenotype so that’s how i would link like the sars causing innate immunity dysfunction and then causing adaptive immunity failure so what happened to sars cov2 specific c4t cells so are they functional so to look at them let’s stand your way to look at star specific or antigen specificity for t cells either you need to have a hoa restricted like tetramer and it’s going to be hard to design for each individual or you use interferon gamma like cytokine secretion but those it’s kind of complicated because you need to fix the cells to look at interstellar cytokines staining but then after that you cannot do rna-seq because fixed cells have very poor quality anyways so shane kraut’s group developed this activation induced markers staining like back in 2016 basically if you have cd4 t cells in the presence of apc or just ppmc you throw into these peptides those like 11 to 15 like or like amino acid kind of little little only cut out like peptide pools then if they’re antigen specific c4t cells they’ll respond to this stimulation just over like 9 to 24 hours of stimulation so if you just sort out cells that are expressing activation markers such as cd69 or the signal 2 of t cell active 6 or receptor signaling such as cd137 or cd154 if you just find these cells that they express these activation induced markers in flow cytometry then you can store them out count them and and answer what’s going on with stars specific c4 t cells so first people found that with in severe patients severe patients you have more cd4 t cells then you have more specific c4t cells so they’re there not only they’re there they’re functional that they proliferate upon stimulation and they express interference gamma so through this detailed single cell analysis now we know that they do have robust t cell immunity but the just the caveat is that these are in covalent individuals that after they recover from from the severe infection they do have robust as memory specificity for t cell response then people started to find out well this is a nice assay but when i look at uninfected individuals or unexposed individuals they also have these like like and like these are specific for t-cells so do they does that mean that other people that are not infected are also protected the answer is uh maybe not that it’s that so there may be some cross reactivity from the common code coronavirus with stars kobe 2 but having these uh like star specific t cell like phenotype doesn’t really guarantee protect immunity it’s just like reflecting that it could be a cross-reactivity with the other coronaviruses but in those patients who are documented to have cova-19 the good news is that the percentage or the number of frequency of such specific c4t cells if you calculate the frequency they correlate very nicely with the antibody titer note that this is the spike receptor binding domain igg these are the antibodies that are most likely neutralizing and this study also has um but neutralizing assays that not only it’s about antibody tighter but it’s also correlating with neutralization so yes cd4 memory uh cd4 help is correlating with the antibody tighter with the very nice correlation so there’s no discriminating they’re going in the same direction which is great then as shane crottie’s crew try to ask so so why do some people especially the elderly have a more severe disease again from all these analysis and looking at clinical data and other things all together they found that something matters called naive cd4 t cells you’re like aren’t we talking about specifics for t cells why do we now talk about naive cd for t cells so it’s like this typically we as humans have 10 to the 11th t cell repertoire saying that we we can recognize up to 10 to the 11 different kinds of antigen stimulation they’re just some naive cells sitting there once the antigen comes such as sars then uh like a few of them where some of the clones will will respond proliferate activate and develop memory and that’s the pool we have we have such a big repertoire to respond to very many different kinds of antigens so it is proposing that this paper that uh when we get older we will lose some of this repertoire you know some fail to be maintained and during the first step of cyto like of the cd4 t cell depletion early infection this may further dampen this some c vertices of reprimand may just be gone because of the cd4 depletion so because we lack the big good repertoire to respond and that may be related to why some older people may have severe coping 19. so if you use single cell methods to look at what these are specific c for t cells are doing they’re actually quite interesting and different when you compare sars kobe 2 specific c for t cells with common code coronavirus or flu because if you look at these the so-called like uh um plot or these dimensional reduction plots in single cells you see that well the the cell type that that stars infection juice looks quite different from those that are singing common cochlear virus or flu so it turns out these are very interesting cells such as t follicle hepa cells you can find here or you can find a cytotoxic cd4 t cells see this is unique and this is only seen in stars but not in chronicle coronavirus and flu so this is very interesting in this paper it seems like well they see during severe cobalt 19 there are more cytotoxic c for t cells and fewer t-rex may be reflecting the overall activated state in this severe infection but we can do a lot of functional analysis using the single cell method so our lab is interested in what’s happening during the early onset so it’s a preliminary study that we took samples from the eo impact study that we look at the sars kobe 2 specific c for t cells we found that these sarcophagus specifically for t cells do develop very early after symptom onset can be as early as the first week we in the process of doing functional characterizations final questions with all these that we learned from from these publications can we develop durable immune responses to cov19 and can we stop the cytokine stored and revert virus-induced immune dysfunction great news coming out this week from shane chronic’s group that they follow up their sars kobe 2 uh pcr-diagnosed confirmed patients including mild moderate a severe copen19 six months later right now more than 90 of the individuals will have good antibody titer igg producing b cells are there and sar specific memory cd4 t cells well we still can’t say that having a titer means totally protective from secondary infection but at least this is promising that you have mild disease severe disease 90 of the individuals you do see these many components standing there ready to fight and you can see this very nice immunology that over the course of infection t effective memory cells when the infection you know goes down to wings the effect of memory decrease but central memory which is your memory that you you keeping your your lymphoid tissue to keep this immune memory start to increase so this is a very exciting and second how do we treat the cytokine storm and immune dysfunction so this is um in the emery by by the bossinger and pertinent group that they tested this in the macaque model as angela said these mecat models are are like mild to moderate disease they don’t the monkeys don’t really die and it’s not really overcapitulate real human infections and they infect charged kobe 2 and started this jack inhibitor by receding two days after infection this is almost impossible in human clinical trials because you know if i get a copy 19 today i may have started coughing three days later and it’s probably going to be a few more days before i get any treatment in the hospital so this is a very short period from virus to treatment but anyways as a proof of concept they’re testing if we block those jack stack pathways downstream of interferon can we stop this systemic inflammation and cytokine storm using this jack inhibitor barista nib so by looking at the monkey lungs and other single cell profiling methods and then the blood cytokine levels the overall finding is that by giving jack inhibitor you can decrease inflammatory cytokine chemokines you reduce the number of macrophages neutral fuel like it’s gonna stuff up your lung and get raspberry failure um you can reduce activated cd4 t cells the great thing is about this is that we had fear that jack inhibitor is somewhat still immune suppressant we want to keep the good interference signaling but we want to suppress the cytokine storm we want to maintain a good um t cell response because we still want the memory preliminary data at least suggested that there this where cytokine jack incubator treatment does not impair c such t cell response and does not really impair the type 1 interferon signal so that is great that so so although it’s still i don’t know whether this can be successful in in humans and i read it from merkel purdue’s twitter is that fda already approved the emergency use of paracetamol in combination with ram deserve the antiviral drug and as as emergency use for cobalt so in summary i would like to thank my lab who maintained our productivity and integrity during this difficult time and this is jack and raja who did our preliminary studies who are still processing those samples this is what they look like in normal times and equivalent times we’re very thankful to be at yale with a very good uh like a clinical and basic science collaborating yo impact study team in akiko iwasaki’s lab her postdoc carolina and mvps student john was provided just like tremendous help for us to to like look at the system and get us involved in the bl3 all right thank you take questions thank you dr ho for that very in-depth presentation so as mentioned it is now time for our q a session and we do have several questions already submitted so let’s get right to them uh first off i’d like to ask dr rasmussen if it’s possible to kind of go over the models that she mentioned and also the models that doctor also mentioned as well why are hamsters and macaques are there any special properties that make them very good or at least popular covet 19 model so yeah that’s an excellent question so some of this has to do with um the the ability of those different model systems to accurately recapitulate human cova-19 disease um and some of it is just really practical so at the beginning of the pandemic it was really apparent that we needed to develop animal models that could recapitulate cova 19 in humans as quickly as possible which is really challenging to do when it’s a brand new virus that nobody’s ever worked with before and you don’t really know what kind of responses you’re going to get in a given host so really what you do is you take the animals that you have in-house that you can you have experience working with and you start infecting them and you you start to characterize those different models so macaques are often one of the first models that are developed for any human disease um just because non-human primates are more similar to humans evolutionarily and oftentimes the fda will also require non-human primate data in order to approve any drugs or vaccines um as part of their so-called two-animal rule so often the the first models that they develop are either rhesus or cinemagist macaques and in fact that’s that’s what happened and my collaborators who actually did the macaque studies at rocky mountain labs which is the nyad uh facility in hamilton montana they have rhesus macaques that they can get and they have a high containment lab that is already set up to do that type of non-human primate work and to do that uh chest x-ray the imaging techniques that i mentioned briefly um so that was it was really a practical reason you have the monkeys in-house you can get right to work um and so that’s why that model was developed but it turned out that in that model while it’s good for looking at mild or moderate disease um it’s it’s really not sufficient for causing uh severe disease and very early on also um people tried to infect laboratory mice that’s an animal model that many people who do animal work have um already in-house but but sars coronavirus ii doesn’t efficiently bind ace mouse ace2 so there was really no disease so people used a transgenic human ace2 mouse and depending on the strain background of the mice you get different levels of disease but then you get the criticism that transgene expression isn’t always uh the same as ace two expression in humans so um people do still use mouse models now there is a mouse adapted virus that has been developed by ralph barrick’s lab i think that people will probably start using in lab mice um so that has some utility but i think really people also tried ferrets early on because ferrets are a great model for influenza particularly for addressing questions related to transmission because their respiratory tracts are more physiologically similar to ours um ferrets will cough and sneeze for example whereas mice don’t so people also tried ferrets but unfortunately ferrets don’t really get sick at all even though they get infected so that wasn’t a good model for looking at severe covet either and that’s when people start looking at some of these other models such as the syrian hamster which does develop more severe disease there are there are benefits and drawbacks to all of these different animal models um so really you always want to to make sure that you’re using the right model to address the particular question you’re asking if you’re asking a question about transmission but you don’t really care very much about the effect on pathogenesis then a ferret model is perfectly fine for that purpose if you want to know something though about what what causes disease to become more severe then you would want to use a different model that actually is susceptible to severe disease so that’s really some of the calculus that goes into choosing an animal model i think going forward there really is a place for all of these different animal models within covid research depending on what type of scientific question you’re trying to address thank you dr rasmussen next for dr ho is there any relationship or correlation between t cell counts or proportions in the peripheral blood relative to their localized infiltrated numbers in the lung or upper or lower respiratory tracts that’s a very good question so for example when we see low c4 accounts in the blood you see oh maybe they are just like being recruited to the lung and that’s certainly possible our data is limited for example in the single cell data in a bronco aviola lavage data set that they see a large increase in cd8 t cells but they didn’t report a large proportion of cd4s so we don’t know whether cd4 are just lost or they’re they’re there but you know bronco villa lavage it’s a levatch so it doesn’t really puncture through the lung and pull it out and look at all the cells in there it’s just washing something from from that for a quick sampling so we we actually don’t know i would say it’s possible that they’re attracted to the infection site such as the lung that’s highly possible but i believe that there are also the direct cytotoxic effects by tnf and then fast license for example that’s already shown that are they’re causing these big drops thank you dr hope we have a lot of uh similar questions about persistent covet the so-called the dub long runners so i’ll i’d like dr rasmussen to begin and perhaps maybe they’ll just be kind of a generalized question how does what we know about the immune response and immune over expression and under expression various circumstances how does that translate potentially to these long runners and these people who have coveted symptoms for months and possibly years that that’s an excellent question and i would say that the the short answer is that we don’t really know um but a longer answer about that is that almost certainly the immune responses um and the inflammatory responses are probably inextricably linked to the the various presentations of so-called long covid um i think that you know long covet itself is something that we don’t really have a good idea of the extent of it i mean there are there are a number of different types of presentations of that that can be very different from one another everything from neurological symptoms the so-called brain fog to symptoms that sound an awful lot like myalgic encephalomyelitis or chronic fatigue syndrome to potential uh lung injury that that is persistent and that might actually be caused by physical damage to the lungs which we know as well that star’s coronavirus classic can induce as well as as mers coronavirus so it makes sense that sars coronavirus ii can probably also damage the lungs in that way um there there have been heart problems reported there have been vascular complications after people have recovered so this is really a very protean condition um that probably you can probably divide people into subgroups um in terms of them having different mechanisms for what is causing you know the umbrella of long coven um i think that you know one question that i have about it is how many of the symptoms are due to direct tissue damage caused by the the virus or caused by the immunopathological responses to infection versus how many are caused by essentially a reprogramming of that person’s inflammatory responses in a given tissue um in particular with the the neurological effects of it i think that you know it’s it’s hard to say if the the virus is actually killing cells in the brain or in the central nervous system i mean certainly there has been infection reported in in neurons and nervous tissue um but it’s it’s very unclear to me if maybe that infection rather than causing direct damage to those cells is actually changing fundamentally changing the way that resident macrophages or resident immune cells are behaving within those tissues and that effect lasts for a long period of time so again my short answer is i don’t know but i will be shocked if there is not a huge component in some kind of aberrant immuno-inflammatory responses in the pathogenesis of long covid yes i agree with what angela said i would say three things the local structure local immunity and false positivity so first the local structure is that if you expect someone have a very damaged lung that there’s a little little bubble in there it’s just like afterwards when this disney is destroyed by bombs it just takes time to really recover so there could be some little niche here and there that the virus is not wiped out because the loads will destruction and second is the immunity that’s likely related to the underlying immune disease such as diabetes or other like aging and others that you need very robust antibody response and then inside the lung to to really clear every single one of them out and then you have cg t cells to kill all the infected cells so every every component needs to be by robust so there may be some people who just don’t have like robust immune responses like in the very first like couple of weeks and third is false positivity like maybe they are still real virus pcr detected but they’re dead viruses they’re somehow already like levels shedding from the dead cells that are not infectious this is possible but we don’t know again the short end is we don’t really know i think doc dr ho you touched on this uh very briefly justin the answer to that last question but i’d also like to ask both of you starting with dr hope do we have any data on covet and immunocompromised individuals who would have weakened immune function and be more susceptible to infection but also theoretically would have lower risk of cytokine storm that’s a very good question and for example so this week i think there is a paper coming out in c cid may be looking at the source infection if hiv infected individuals i haven’t looked deeper into that paper yet but this is something interesting and there are other specific disease groups you know but even in diabetes for example the immune status of diabetes patients is a range of the spectrum of immunity so i would say uh the immune compromised status will affect uh viral control but as what um nation chronic data show that majority of the patients in any part of the patient that that they they profile ninety percent of them develop good memory t cell results and antibody tighter so i wouldn’t say that 90 of all these people are all healthy they must have some underlying but they can still develop good immune responses dr i’ll just add to that um that recently a couple papers have come out describing an individual patient um i believe both of them were either you know they had a hematological malignancy they had i think lymphoma in one case in another case it was a patient who was undergoing treatment for cancer um those are certainly both patients who would probably be immunocompromised or immunosuppressed to some degree and there was persistent infection reported in these patients um now we don’t have evidence that persistent infection is happening in everybody but it certainly seems plausible to me that as dr ho was just saying you know if if a patient is immunocompromised there may be issues with actually clearing the infection itself so it does appear that being immunocompromised in some way may affect the ability to clear the virus whether or not that relates to disease severity over the course of their infection um it’s it’s really hard to say with the number that that we’ve seen the number of cases that have been reported um but it’s certainly something to look into in particular i think looking into that with regard to hiv patients where there is a huge population of hiv patients um taking drugs that control their hiv will have varying degrees of immune suppression i think it’s it’s a really important question to ask and that’s in fact why hiv positive patients were also included in some of the vaccine phase three clinical trials um to make sure that those vaccines could perform adequately and provide protection in those patients uh but that do have hiv at least um but immunocompromised immunosuppressed is actually a very broad term that can refer to a variety of different conditions um that that may be you know different in terms of the mechanism of the immunosuppression so it’s really hard to generalize about this but it’s it’s definitely an area that we need to take a closer look at thank you both for those responses i think we have time for one let’s not call it a question let’s call it a topic of discussion and we have quite a few audience members wanting to know if there’s any any correlation or any relationship between symptoms severity and the robustness of post-infection memory development and i want to let dr rasmussen answer first please yeah so that’s a really good question and i again will say i don’t really know the answer um but just in general uh i think that robust immune response to the virus um you know in general both innate and adaptive immune responses are associated with more rapid resolution and less severe disease i think though the the associate i mean disease severity as dr ho had spoken about um in her talk disease severity has been linked to some of these various uh depletions of certain types of t cells um you know the t follicular helper cells and the germinal centers that both of us talked about things like that but across the board i’m not aware that we’ve found the you know the smoking lymphocyte uh to say to use that term um the the smoky lymphocyte that proves that you know if you have fewer of x cell um or x cellular responses you’re going to have more severe covid no matter what i think it’s it’s a really complex question and and dr ho did an excellent job of showing exactly how complex especially the adaptive immune system is um so again short answer i don’t know but i think that’s something that we do really need to look into um as it does have implications as well for things like biomarker development how could we better triage patients who who might need one treatment or another or who might need to be hospitalized versus not um i think that it’s a it’s a really important question to ask and we need to to be looking harder at predictors of disease severity uh yes i agree with what angela said i will add a few more comments so first there um those high dimensional analysis papers say akiko iwasaki’s paper and john warwick’s paper they many of those people take all these clinical parameters including fever underlying comorbidities obesity like hypertension and many many like disease scores into consideration um into you’ll see those many very colorful heat maps that they are also trying to figure out that what’s the best marker to predict severity or immune response so they all have those beautiful plots but for what dr akiko iwasaki’s paper showed is that well they named the interferon is one of the marker that is indicating disease severity there are other like cytokines that they named but specifically for fever for example typically we think if i have a fever today i would think this is the reflection of an interferon response either i get a rhinovirus or get a covalent anything so interference response having fever yeah that’s sort of what i would think but in kobe 19 is messed up see the cover immune response is complicated and we know that covet you don’t need to have fever you can still get infected it’s it’s too late and too little so i may have a bad disease but i don’t have a fever and second thing is that there are always a clinical observation that older people or immunocompromised people they don’t develop fever for example if i am autoimmune disease i’m taking immunosuppressants such as long-term steroids i may not have a fever but but it’s just i don’t i don’t have this fever but i have a very bad disease going on so it gets very complicated to say if fever is a predictor of memory response it usually usually is for example the classic animal model example yes but in colbert it gets very complicated related to that and the answer might be we don’t know again but is there any correlation then between symptom presentation and immune time course immune activation progression well i think um dr ho had a really nice figure um in her paper from that recent review by mood civic and colleagues showing that you know virus load peaks often before symptoms become completely apparent um and this is one of the reasons why the pandemic itself has been so difficult to control um but i’d be very curious to hear dr ho’s answer on this about timing of the various immune responses because generally in my work um for sars2 or any other emerging virus a delay in the innate response does impact symptom severity um but i’m not sure that we have a great answer to you know is this conclusively determining symptom severity in terms of you know when x immune response goes up um and the type of disease that a person will have yeah i agree this is a complicated question but usually symptoms should represent um like viral load interferon again this is disconnected in the in the sense of covet when we learned this from the example of hiv for example hiv may have like viral early peak of viral load but if we treat patients very early before they really pee you start treatment that really restored all the immune responses so i would take it into a different answer is that if we have um like like star symptom onset that if we get some early treatment say really early and death severe or early kind of antivirals just like you take tamiflu and the first 24 hours of influenza or you take a secular year in the first 20 like 24 hours of herpes zoster that they can probably change the disease course and ameliorate symptoms but like things after three five days is getting complicated between the battle of the immune system and the virus and there’s a question in the in the in the chat saying that why don’t we use like inter interferon alpha spray in stars cov2 i actually don’t know because that was provided immersing factions for healthcare workers they just have a interferon alpha like nasal spray to prevent but i don’t really know the administrative part that why we don’t try this in our school so dr dr ho i can actually answer that i think that those trials are going on right now um i think the issue is that and this is just what i’ve heard um from ben 10 over i believe that uh you actually can’t use interferon as a true prophylactic um just because repeated administration intranasally um causes like the mucous membranes to dry out it basically um it it messes up barrier function and i guess it’s just pretty uncomfortable but i don’t really know and i think it is in a clinical trial right now i don’t really know why they’re not treating patients at the time of diagnosis especially people who are asymptomatic with interferon um intranasally or potentially i well intranasally would be the way to do it i guess or nebulized but um i think that those studies are ongoing i just don’t think we have an answer and i think that some of it has been a little bit people have lost their enthusiasm because of the results of the solidarity trial which was using interferon in hospitalized patients so that i completely agree that it’s going to be less likely to work in those patients just like rem deserve and just like monoclonal antibodies are because as you pointed out um that by that point you’re not really fighting against the virus you’re fighting against uh the the immune response or the dysregulated inflammation sure i i totally agree i think what we know about interferon is that timing is so important so you cannot give it like so seven to ten days if you give it that may be the culprits leading to leading to severe disease so timing is so tricky [Music] thank you very much to both of our speakers today unfortunately that is all the time that we have if you have any further questions please consider reaching out to the speakers directly and their emails are presented on the screen i would like to thank everyone who took the time to join us today especially those of you who shared your questions and your comments and on behalf of the scientist i’d like to extend a heartfelt thanks to our speakers dr angela rasmussen and dr yachty ho as well as our sponsor bps biosigns thank you everyone and have a pleasant day