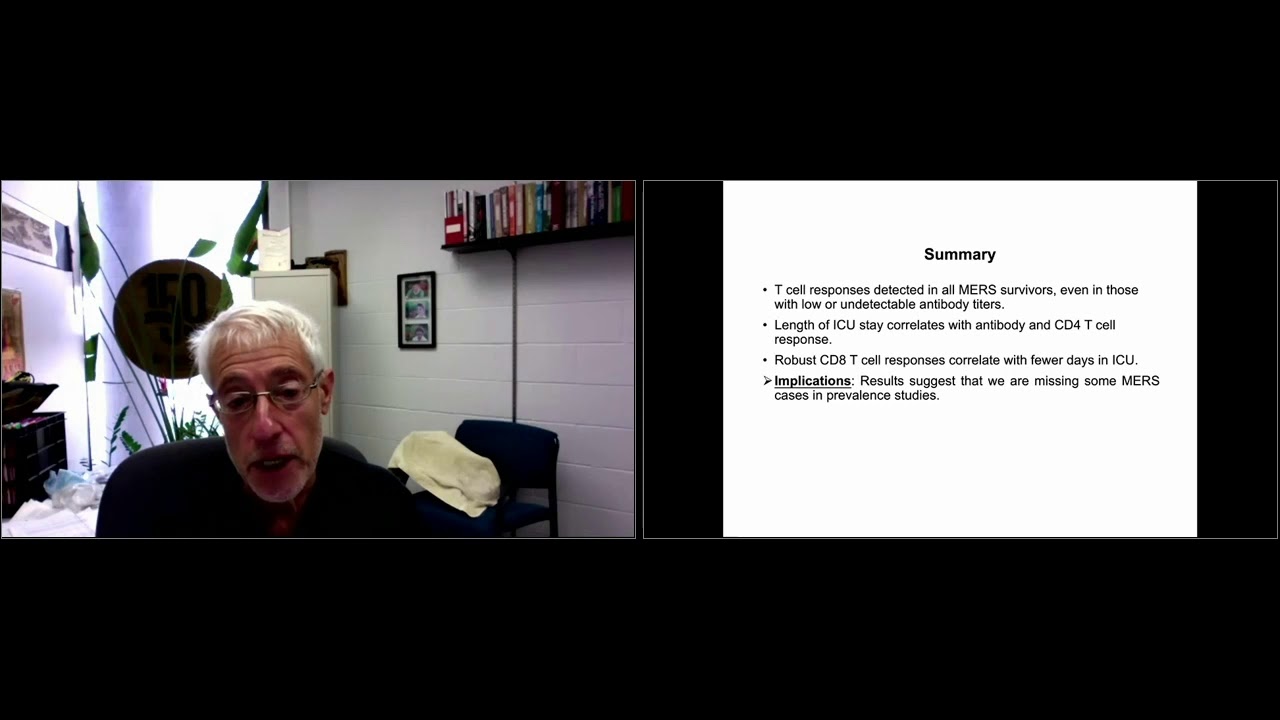
Stanley Perlman, M.D., Ph.D., discusses the immune response to the SARS-CoV-2 virus during ASGCT’s COVID-19 Symposium.
so i’m going to talk about the immune response to the virus and i’m going to start by describing some of the things we know about the immune responses then the latter part of the talk will be about some of the illustrations we have from my lab studies and other studies of when the virus immune response actually is deleterious and of course this is relevant for covet 19 because there’s lots of evidence that much of the disease is actually the immune response to the virus we’re still working out many many of the details there but it seems as the virus replicates and the host responds there’s this regulation of the immune response and it causes many of the pathological findings that we see so just i think some of these things may have been covered a bit already but there’s four common cold uh coronaviruses two two nine eight hku1 and l63 and oc43 oc 43 and 2298 have been identified for oh probably about 40 or 50 actually more like 50 or 60 years now hku1 and nl63 were identified after the sars epidemic in 2003. they cause up to 15 to 30 percent of common colds and one feature of them is that there’s no durable immunity there’s frequent cycles of infection and the more we know about of course about covet 19 this is a characteristic that both occurs and is something we worry about upper respiratory infections are most common lower respiratory infections are uncommon but they occur in aged immunocompromised patients again a common theme of what we’re seeing with covet 19. these viruses all like to infect the lungs of people who are more susceptible or have some underlying morbidity or aged and of course there’s no antivirals or vaccines for the common cold coronaviruses and the comet what we know about immunity is that many of these viruses induce an antibody response but the antibiotic response either wanes or is transient but i think it’s the best study is one from 1990 from the cowardly towel where they inoculated 15 volunteers with 229e 10 of them with lower antibody titers became infected in eight developed colds a year later they challenged this group nine became reinfected and there was virus shedding still we don’t know how much virus shedding and this is of course important as we think about vaccines in the context of covet 19. none of these nine people developed the colds however so so from this we can say common cold coronaviruses do induce an immune response it’s not durable but it lasts for a while and it does protect against developing disease and we we know something about vaccines from previous coronavirus infections as well most of these are in domestic and companion animals so before people started thinking about coronaviruses in humans the main interest of these viruses was in the disease they caused in either companion animals or in or in food animals or domestic animals so we knew one of the diseases that we knew something about was feline coronavirus which is normally a coronavirus that causes diarrhea in cats but then every now and then it mutates while within the same host while the host is persistently infected to become feline infectious paranitis virus and this virus is uniformly lethal and one of the things that makes it lethal is that instead of being just a normal diarrhea virus it now is able to infect macrophages and this is fairly unique among coronaviruses not completely unique but fairly unique and because of this this is the only illustration of antibody enhanced disease this is something again when people are thinking about vaccines there’s a big concern that that there’ll be antibody enhancement this occurs in feline coronavirus but it may be the only example of this ever occurring in a coronavirus the ones that we are most concerned with now uh in human populations uh sarsko v2 and in 20 years ago sars and murskovy do not productively infect macrophages except occasionally for merscovy and then another illustration of vaccine is transmissible gastroenteritis virus which causes fatal diarrhea newborn pigs people had worked on for years trying to develop a vaccine for this virus and they there was some success it took a while to figure out what you needed was an iga response in in the milk of the mother pig in order to protect the baby but it turned out nature figured out how to protect figs from this virus a virus naturally arose that was changed in just one area of the spike the surface glycoprotein and it no longer could bind to the entire track it only could bind to the respiratory tract and mostly the upper respiratory tract so the result was this was a great immunogen and it basically eliminated the virus from pig populations and one consequence was that investigators actually working on tgev had to find a new virus to work on because there was no more tgv this is really a great illustration of how vaccination can work in coronaviruses and we know from mouse studies from my lab and others that antibodies are protective they can be delivered passively if given one day prior to infection and this this may be relevant for understanding how convalescent plasma works or even more if we ever get to a cocktail of monoclonal antibodies which i know are in clinical trials now we know the virus specific t cells in the absence of antibody are partially protective we also know that vaccination with live attenuated virus is the most protective way of immunizing animals that’s shown again by the tgev pig study that i described in the last slide so the antibody responses in coronavirus infected patients we know that neutralizing antibodies are critical for protection against re-challenge are they the only part of the immune system that does this probably not because t cells matter too and t cells do provide some protection uh antibodies and merge survivors waned uh rapidly especially those with mild disease and this is very so common in what we’re seeing with covet 19 now the more mild the disease uh you may get an antibody response but the more likely it is to be transient or to wane over the next few months and of course one of our goals with vaccination is to make sure that if we have a vaccine that there’s not a substantial waning some of the studies with the mers vaccines using the same platforms as are being used for covet 19 suggests that waning does occur uh whether this is going to affect the long-term long-term protection is still unknown but there’s certainly evidence of waning even in that circumstance and on the other hand thesaurus patients start most people got sars got severe disease there was very little evidence for asymptomatic disease with sars an initial study said that while the antibody responses can’t be detected after six years however more recent studies show that all levels of antibody can be detected for up to 12 years and my lab in conjunction with ginseng zhao’s lab in guangzhou has detected virus specific neutralizing antibodies in 16 of 18 sar survivors at the 15 15-year mark so this again supports the idea the more severe the infection the more likely you are to have a long-lasting antibody response but these patients i don’t know how severe the disease was i don’t have that information so this just repeats uh what i just said uh just notice that the antibody tires are pretty low they’re between one to eighty and one to one forty for protection in humans right now we don’t have a really great number but the guess is around one to two hundred or one to may be required for protection so we don’t really know if these people would be protected from cyrus covey again we know there’s some cross reactivity with sarsko v2 but it’s probably not going to be sufficient to be very protective but maybe it’ll do a little bit and then there was also some cross reactivity with murders covey so this this is a slide that i did uh that my lab did with our collaborators in saudi arabia with the beer auschwitz and looking at the yellow buck or orange yes orange box area you can see that these patients had just pneumonia not severe pneumonia but mild pneumonia and they initially had a positive elixir antibody tighter and we like to do neutralizing titles but they were not done in this study and the neutralizing tires were detectable at three months had weighed by 10 months and then by 18 months they were no longer detectable whether they be detectable by neutralizing titers i don’t know we were able to in many cases detect neutralizing titers in uh murders patients who no longer had elisa positive titers so this is this part is not completely known and so because of these questions of antibody responses we began to investigate t cell responses and as i mentioned earlier cd4 and cdat cells are critical for clearance of infected cells and when we started this there was nothing known about t cell responses in mers and we as i mentioned how long antibody responses were detected in patients who had had sars sars cov specific t cells were identified as long as 11 years after this after the infection and again in conjunction with jin sun jiao we found that t cell responses were detected in the same survivors and uh this there was and one point that’s important is that there was no evidence of mers specific t cell responses in uninfected humans i say this is important because this particular issue has confounded our studies of sars co-v t cell responses as i’ll mention in a minute so just to summarize this part t cell responses were detected and all murder survivors and the length of i this i didn’t show this but in published work we showed that the length of icu stay correlated with antibody and cd4 t cell responses and this is a consistent with the idea that the more severe the infection the more likely you are to have a robust and long lasting antibody and t cell cda t cell response robust cd8 t cell responses correlated with fewer days in the icu i skipped over a point but it’s they were also in patients who died they often had high cda t cell responses but that this is in survivors so it’s a little different scenario so one implication of all this is that because we usually measure antibody tires particularly biolysis that we’re missing some cases in prevalence studies so what we do now is we we tend to measure uh wheat pen to measure neutralizing antibody titers in all our patients i didn’t show the data for that but because we detect more patients using this method this is our method of choice for identifying infected patients for sars cov2 it seems like our elisa tests are better there’s so many more of them there was only one uh mers or one or two mers antibody tests and they they were i think fairly specific but not so sensitive so another issue is that uh the t i mentioned already this pre-existing immunity to covet 19 is confounding studies of the t cell response so there’s several studies now that show that you can detect saris cov two specific t cells using activation markers so this you stimulate cells with peptides specific for the virus proteins and instead of measuring functional breed outs like interfering gamma production you measure activation markers and the issue with this is that we see a lot of the people doing they see a lot of us people having responses to uh cyrus cov2 proteins and it’s hard to know what this means activation markers are not specific so but there’s something in the media that’s activating the cells and whether it’s truly cross-reactivity or what it means is really unknown we don’t know if they’re protective they’re pathogenic but they are confusing and it’s this is an area that definitely needs more work as we try to figure out why mersco v had no cross reactivity cyrus cov2 seems to have a fair bit of cross reactivity and it’s not it’s not against usual proteins for the most part that are seen in the normal source cov2 immune response it’s some of the non-structural proteins this is definitely a work in progress so uh the furcovit19 t-cell responses uh we know from several studies now that they’re directed against all the structural proteins and also some non-structural proteins as i mentioned earlier some of the just now in fact some of these responses to structural proteins are hard to understand they’re they’re not usually seen to great levels in covet 19 patients and they also don’t cross-react with the common cold or seasonal coronaviruses so we don’t really know what they mean and where they came from and sometimes we can detect even in cyrus cov2 t cell responses in some patients who lack detectable antibody titers one of the one of the goals that we’re pursuing is trying to identify specific hla restricted epitopes so this would allow us to screen populations with a single pool of antibodies of peptides rather and this would perhaps allow us to better characterize the t cell response and we’re solely working up to doing that this field is so uh intense and so intensely studied now of course or there’s so many people in it that by the time we get going on what we do that may be done by seven labs but we’ll see and the t cell response is also important for measuring uh vaccine efficacy especially given some of the results we’ve had showing that t cell responses are more long-lasting potentially than antibody responses so one minute on back vaccine enhanced disease this is a of course a big concern with vaccines coming on the market now other than feline virus which i mentioned earlier there’s no evidence of macrophage enhanced ade or antibody disease enhancement but there is though is there’s evidence from several studies in the past of changes in the character of the immune cell infiltration this was seen when inactivated whole viruses used it’s seen more in aged mice associated sometimes with eosinophilia i should say that none of these mice get sicker because of this these are histological changes or pathological changes not necessarily reflected in clinical disease and there’s one study in macaques that showed that immunization with a vaccinia virus expressing the s protein or taking antibodies from those bison and giving them to a second mechax and giving to a second macaque before infection with sars cov2 there was a change again in the nature of the inflammatory response it went from macrophages went from wound healing to pro-inflammatory and there’s increased expression of inflammatory mediators but as in the other studies the macaques that didn’t really care they remained asymptomatic so this is something as we i’m on several committees that discuss vaccine safety and this is something we think about all the time it’s very hard to measure distinguishing these kind of enhanced respiratory disease problems versus vaccine failure so i’m going to spend the last seven minutes here on talking about when is the covi immune response pathogenic so i’ll start with it by reiterating the vaccine studies that i mentioned above where at least in the case of feline coronavirus if you immunize with the surface glycoprotein under certain conditions you can get enhancement of macrophage infection this of course is the same as seen in dengue virus infections and this but this is the only illustration really of a pathogenic immune response that gives horse disease i will show a little bit about mouse hepatitis virus induced demyelination because it’s a subject that i’ve studied for many years and i think is gives a good illustration of possibilities and then i’ll talk for the last couple of minutes about dysregulated early immune responses which i’m going to show our data from sars from a few years ago rather than kovac 19 which we are still in the process of doing and what i should say is that what we know from covet 19 patients is that sometimes the immune response the interfering response is delayed or absent other times it seems to be present and remains present for a long extended period of time so how this is exactly all playing out is unclear whether it’s a failure to reduce an interference response or a failure to do do so properly regulated interfering response was people are still trying to figure this out this of course is very important because if somebody has a delayed or absent interfering response they might respond to exogenous interference and as i’ll show in the next few slides you wouldn’t want to do that necessarily too late in the infection because it might have negative consequences so this is the mouse hepatitis virus slide and i’m only going to show you the single slide the point of this slide is just looking at the second row here let’s see if i can get this to work yeah so this row this is a mouse that’s infected with mouse hepatitis virus and this panel here shows that there’s lots of virus antigen in the white matter these are all infected oligodendrocytes and this is myelin and it looks basically normal and this is axons running through the myelin again looking normal and these mice have no t cells which is why the virus is just infecting these cells and nothing much else is going on now if you take these same mice and give them t cells and wait a week you now have complete destruction of the myelin you have macrophage infiltration to a huge extent and now the virus is cleared so this is one of the things that’s really interested me as paul had mentioned over the many many years how come the virus how come the host cannot clear this virus without causing so much tissue destruction and this may be relevant for our understanding how the human pathogenic respiratory coronaviruses work so uh one a study that we did a little while ago was looking at interfering in mice with either sars or mers and mur as type one interference are the mainstay initial immune response and they’ve been used both prophylactically and therapeutically and various infections so we think it’s really important to understand how what they do and how they do it so one of those things that this my postdoc who did this uh chana pandavar who’s now a pro assistant professor at the university of tennessee what he was able to do is he was able to take a bouncy mouse that normally gets quite sick with this virus huge weight loss death and now if you infect a interference knockout mouse on the same background lice completely survive so this was our first hint about how interferon responses could actually be pathogenic and the other thing that he should that he showed was that when you took away interfering you actually didn’t change virus clearance very much this may be a slight delay at day three but by day five there’s no difference in virus clearance the other point of this slide which will be important for the next slide is that the virus titers are almost reached maximal levels at 16 hours post-infection they’re slightly higher 24. and for anyone who works with other respiratory viruses this is hugely fast and hugely high and one of the things we notice is that the interference response lagged so here the the response is 48 hours peaking yet we saw virus speaking at um 14 at um 16 to 24 hours so this we thought might explain some of the pathogenesis all these other factors also peak later ccl2 and tnf which were important cytokines and uh chemicals and then what rouge was able to do is if you deliver interference six hours before the infection and so taking away this lag now mice were completely protected and they survived and they lost much less weight so again supporting the idea that the timing of interference is really critical for uh in relation to virus titers to predict outcomes and so now going to a second virus i’ll come back to put this all together in a couple of minutes but if you get inverse the opposite was true so interfering with protective if we took mice and now infected interfere knockout mice now they all died that showed in the red box area and virus clearance was also delayed and then but here here’s the i thought was a piece of slide that gives us some information about what’s going on here the virus titers peak at two days and interfering peaks at two days so there’s none of this lag that we saw with sars and then what we could also show here is so now if you treated if you gave a lethal dose of virus and at six or 24 hours before infection now mice didn’t lose weight and they would completely protected or not completely almost completely protected in terms of survival and virus was also cleared much more rapidly these are the interference treated mice you can see here it’s particularly obvious here so interferon again preceding the virus infection was protective and on the other hand if we mimic the tsar situation and let virus peak and then gave interference now we saw we could we had a lethal outcome so this is the mice this is with a sublethal dose of myrrh so mice would not die or a few of them die that’s shown in the blue and in red when you give virus either two days after infection or four days after infection uh you have a great decrease in survival much more mortality so and the same thing is true in sars if you give a sub-lethal infection where a few mice die you give interference during the infection now they all die so the basic point of this is that it’s really important that we know the relationship of when the into the immune innate immune response and the virus are work are functioning compared to each other uh what what these mice experiments show is that it’s really key that the interference response as much as possible precede the peak of virus replication and we know from sars in 2004 that patients who did poorly many of them not all of them some of them had no interference response but many had prolonged type one interfering expression and when this was shut off antibody responses developed and patients survived and so this is important for thinking about the use of exogenous interferon in kovi and other acute infections so i just want to thank rudra who china panama who did most of this work my long-term collaborator your fearless moderator paul mccray kunlee and then jin soon and jinxie and joe so thank you thank you stan we’ve got several questions here um see if we can knock off a few uh the first one is is it understood by which pathway feline coronavirus infects macrophages think it’s by through its receptor uh which it’s a good question because i don’t i’m pretty sure it’s through its receptor which is apn um aminopeptidase and protein i know the enhancement is via the fc receptor but i i’m pretty sure that this the two together are required okay a second question uh related to animal models are are you surprised that sars kobe 2 is asymptomatic in rhesus macaques well sarsko v2 is a pretty mild in about 80 percent of humans so i think i don’t think we understand pathogenesis very well yet it’s the ten or twenty percent who get sick with uh cyrus cov2 that that we’re concerned about not the 80 percent who have mild infections or have colds i do not know why rhesus macaques are resistant to this or get very mild disease but you know there’s common themes here because they’re they get mild disease disease after sars covey after mersocovi after uh sars cov2 and we also know that just like in humans uh children do not get severe disease for the most part with sars kov2 saurus covey or mrs covey so there’s some common themes here about pathogenesis that we that are really probably key to understanding how these virus work and why they seem to particularly infect and cause disease and people have underlying conditions or are older another question considering that cobit 19 is an inflammatory disease maybe the vaccine could exaggerate the immune response and you could have adverse events do you expect immune damage from vaccines well this is this as i mentioned during the talk this of course the thing we’re all worried about that is going to be some adverse effects so far in all the people who’ve gotten either the mers vaccines or phase one phase ii trials of the cyrus cov2 vaccines but what i’ve heard more about than anything else is sore arms so local effects that are not uh not particularly worrisome in terms of worse disease that’s one of the things we’re monitoring and this is a key thing to try to figure out vaccine failure from horse disease and so i don’t think we know yet how this is going to pan out okay um thanks another question um how do cancer patients behave when infected by cobit 19 especially patients who go through car t treatments is there any knowledge there there’s not much there was originally it was thought that people didn’t who had who are actually immunosuppressed didn’t do as poorly as other people but in fact now um if we think that immunocompromise is a risk factor for more severe disease i don’t know specifically about people who are getting car t therapy how they’re responding to this you certainly could imagine that you get i don’t know because you can imagine some protection you can imagine worse disease and so you just have to look at the data and see which it which it is uh a last question uh dexamethasone is being used successfully to treat severe cobit 19 patients what are the implications of this treatment in the development of efficacious or friendly humeral and cell mediated immunogenic responses yeah this is i don’t think we know the answer to the yet this is always a concern that if you dampen the immune response uh too effectively that you won’t develop adaptive t cell and b cell responses so i think this is still something we’re still learning about i think the use of storage is an interesting phenomenon because we when it was used in sars it actually led to worse outcomes but that’s because it was used at all times during infection and now it’s being confined to people who are sick in the icu where their inflammation is clearly uh contributing to worse outcomes so it’s really i’m really pleased to see that it actually has a role there i was very worried that it was going to be like sars and lead to worse outcomes but here when virus loads are going down and people have clearly inflammatory disease it seems to be working but i don’t know what the effect will be on the uh ultimate immune response okay well thank you for a great talk and thoughtful answers to these questions