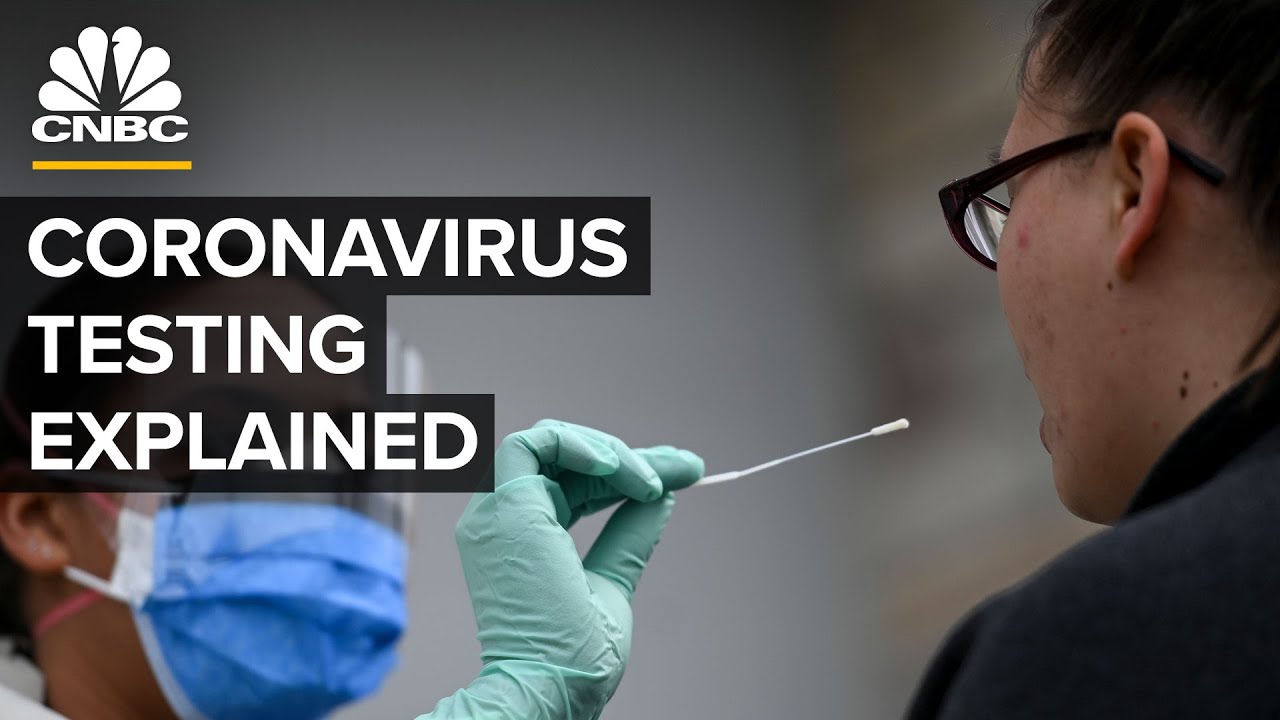
There are three types of Covid-19 tests: genetic, antibody and antigen. More than 630 distinct tests are commercially available or in development, and some major players include Abbott, Roche, Thermo Fisher, LabCorp and the CDC are involved. CNBC explores how each test works and how to know which one is best for you.
» Subscribe to CNBC: https://cnb.cx/SubscribeCNBC
» Subscribe to CNBC TV: https://cnb.cx/SubscribeCNBCtelevision
» Subscribe to CNBC Classic: https://cnb.cx/SubscribeCNBCclassic
About CNBC: From ‘Wall Street’ to ‘Main Street’ to award winning original documentaries and Reality TV series, CNBC has you covered. Experience special sneak peeks of your favorite shows, exclusive video and more.
Connect with CNBC News Online
Get the latest news: https://www.cnbc.com/
Follow CNBC on LinkedIn: https://cnb.cx/LinkedInCNBC
Follow CNBC News on Facebook: https://cnb.cx/LikeCNBC
Follow CNBC News on Twitter: https://cnb.cx/FollowCNBC
Follow CNBC News on Instagram: https://cnb.cx/InstagramCNBC
#CNBC
How Covid-19 Testing Works
There are three types of Covid-19
tests: genetic, antibody, and antigen. But how do they work?
And what’s the difference? We’ve heard sort of test, test, test. What does it mean? What
are we actually testing? Covid-19 is a disease caused by
the SARS-CoV-2 virus, which stands for Severe Acute Respiratory
Syndrome Coronavirus 2. It’s related to the almost
50 other coronavirus species. And right now there are over
630 SARS-CoV-2 tests commercially available or in development. Molecular tests
are the gold standard for Covid-19 testing and are the ones
you’ve probably been hearing about. They’re both the most reliable and
the kind that was first developed. They involve looking for genetic
material from the virus itself. You need to get some of
the virus and some cells. And that’s done by putting a swap right
to the back of somebody’s nose and then taking a scrape. Then scientists take that sample and
run it through a process called amplification. If SARS-CoV-2 is present in
the sample, it’s not enough to accurately study. So this step copies the virus’s genetic
material over and over until there are millions of times more of it
and it can be conclusively identified. The technique most tests used to
do that amplification is called a polymerase chain reaction, or PCR, which
has been around since 1985. So it’s not a new technique, but to do
it with a new type of virus, you need that new
virus’s genetic sequence. And on January 12, China sequenced
SARS-CoV-2 and released that data publicly, which meant that scientists had all
they needed to make a test for it. As soon as you know the viral
RNA you can develop a test for it. So the first plus is you can
develop the test very quickly, almost overnight. And that
happened with SARS-CoV-2. Tests were developed within days of
the virus’s sequencing in January. The question that I think everybody has in
their mind is if it’s that easy to develop a molecular test, why
are we still talking about inadequate testing? Development of the tests is
just one part of it. The whole system that needs to be in
place to be able to receive these tests, use them and so on, is a
much larger issue that goes beyond just the actual physical test. So even though every country and
leaders of every country have promised volumes of tests and all these things,
often they’re looking at it from a perspective of, oh I have access to
XYZ manufacturer and, you know, so many tests and so on. But it takes
a lot more than just the actual test. In the United States we’re still working
to catch up when it comes to getting sufficient tests out there. But hundreds of these
kinds of tests exist. Some of the biggest producers include
companies like Roche, Thermo Fisher, LabCorp and Abbott, as
well as the CDC. If you think you have Covid-19 right
now and you have symptoms, you should take the molecular test. And if you’re in the symptomatic
stage you should certainly have virus that’s enough there to detect. And there are also genetic tests that use
this same basic process but in a miniaturized form. What we’re seeing now
is some extensions to that kind of test, which is taking all of
the machinery that you would normally use in a lab and kind of using a
miniaturized version so that instead of in a lab where we can look at thousands of
samples at a time, it’s doing it just on small numbers of samples,
maybe even one at a time. One such rapid test that has
received significant attention is a SARS-CoV-2 test made by Abbott to work with
the company’s existing ID NOW system, which was already being used to
test for other infectious diseases. ID NOW is really set up for point of
care right at the site of the patient. That instrument is designed to use, for
example, a nasal swab or oral swab and then directly put the swab into
the instrument and perform the test. It’s meant to be used at
urgent care clinics, physicians’ office labs, emergency departments and retail settings; and
tests one sample at a time in five to 13 minutes. Which is great if you’re one person
needing results quickly, but much less efficient if you have a large group of
people who all need to be tested. And there are a couple of studies that
have yet to be peer reviewed but suggest ID NOW’s accuracy may be as
low as 48%, something that Abbott disputes. The more standard lab based
counterpart to Abbott’s ID NOW system is the company’s
m2000 RealTime system. A laboratory instrument, you can
process many more samples. For an m2000 platform, run at optimal
efficiency for a 24 hour period of time, you can analyze 470 specimens. So, much higher throughput. So it’s not like one size fits all. And just because there’s one test that
seems on the surface of it that they are going to solve
every problem, they’re not. The other kind of test that you’ve
likely heard about is an antibody test. When a harmful virus is introduced
into your body, your body reacts. Studying that reaction is another
way to detect SARS-CoV-2. Symptoms or not, if your body has
been fighting the virus, there should be evidence of that in
the form of antibodies. This kind of test uses your blood
instead of a swab from your throat. So this is not directly measuring the presence
of the virus in your nose or nasal cavity. What you’re doing is
measuring through a finger prick or through a blood draw, you’re trying to
say is an antibody response present in a particular individual? There are
two types of antibodies that are produced after an infection. One, IgM, shows up in about
a week and then tapers off. And the second, IgG, shows up after
about two weeks and sticks around for much longer. This adds to the
difficulty in making a consistently accurate antibody test. You could be either too
early in the infection for the IgM to pick up or you could be in the
bit between your IgM and your IgG being detected. Or you could be somebody
who isn’t making those particular antibodies and won’t be
detected at all. We don’t know enough of this particular
virus and genetics and so on whether it lasts a month, six months,
a year, two years, we don’t know that. All of this means that
it’s tricky to develop these tests, especially during a pandemic when they’re
needed much more quickly than usual. In the case of the
IgG test, this was an unbelievably compressed development cycle. Under normal circumstances our
development cycles are years. In this case, the IgG test was developed
in the span of about 30 days. So how do you get a supply chain,
determine methods to be able to scale and ramp to go to
literally millions of tests? Because we could have the best test in
the world and if we can’t produce it, it isn’t getting the job done. Abbott says it will ship nearly 30
million tests this month and will have the capacity to ship
60 million in June. We also don’t yet know what
the consequences of having SARS-CoV-2 antibodies are. It could mean a resistance or immunity
to Covid-19, or it could mean neither. We know from other coronaviruses that
it is very likely that as soon as you have gone through
an infection, you will also acquire immunity. But this still nevertheless has
to be proven over time. The antibody tests become much more
useful on a population level later to find out how many people were
likely infected in the first place. They’re not really a great way of going,
you as an individual are okay to go back to work or you’re
protected or something, because that’s just based on stuff we just
don’t even know about yet. And the FDA recently tightened its
guidelines for companies wanting to sell antibody tests after initially allowing them
to be sold without evidence they actually worked. Ongoing research into
these early tests, which has not yet been peer reviewed, has
shown a troubling lack of accuracy. But there are more than 120
antibody tests already on the market. The one we will be marketing or
distributing is a pinprick test which can be taken and results received in
about 15 minutes without an instrument. Having said that, it is not
approved by the FDA, per say. But we also know that some
people don’t make any antibodies. People can test negative so they
don’t have antibodies, but they could still be actually infectious. Spain and the UK in particular, they
were going to roll out millions of these tests and they’ve ended up
having to abandon all of them. Finally, there are antigen tests. The sample comes from a throat
swab, just like the genetic test. But you’re looking for evidence of
the virus via a completely different method. A rapid strep test that you would
do in a doctor’s office is an example of an antigen test. As the virus secretes proteins called
antigens, you can detect those also. While the end product could potentially
be very simple, developing them comes with obstacles you don’t have
when developing a more straightforward genetic test. First, you need to
have access to the right patient population, get the antigens. You need to then have a way
of immunizing some other animal to develop antibodies, because the antibody ultimately is
what goes on the plastic that you have and what you’ll see even
today is that there are very few true antigen-based tests that
are available for Covid-19. The advantage molecular has is that
you can amplify the genome. So in any of these molecular tests, we
might go from a few virus particles to billions of virus particles
after the amplification step. Antigen assays don’t
have that advantage. But if they can be worked out,
antigen tests could be one important tool among many in the
fight against Covid-19. Just last week, the FDA
granted emergency authorization to Quidel Corporation for a new antigen test
that only takes about 15 minutes. This test tests for antigens that
the virus produces in the blood. So it has antibodies effectively on a
stick and you swab someone with that stick. And then you put it in a
little machine called a Sofia that’s about a thousand dollars. The test itself probably is going
to cost about five dollars. Now, the problem with it is
it’s only about 85% sensitive. So that means if you have 100
patients with Covid come into your office, you’re only going to catch 85
of them with this test. The biggest obstacle in developing any of
these tests has been how quickly it had to be done. So while
there are hundreds of tests already available, it’s unclear how well many
of them actually work. The Foundation for Innovative New Diagnostics,
or FIND, is a global nonprofit based in Geneva working to
bring clarity to exactly that. What we set out to do was set
up a platform where we can uniformly address the tests and see how well do
they actually perform compared to each other and also in terms of
what the needs actually are. That way we can inform the countries
when they look for different tests and how good they are, essentially. FIND currently lists over 600 SARS-CoV-2
tests as commercially available or in development. But not all of
those are being made by established companies like Abbott. And there are new
tests coming out all the time, including at home tests that you would then
send off to a lab like Quest Diagnostics’ recently announced at
home antibody test. LabCorp also has an at home test. Yesterday, we announced expanding access to
our Pixel at home kit. We have over 200,000 kits available
and yesterday we announced that it’s available for anybody that
meets the CDC criteria. This is truly an unprecedented situation in
terms of how rapidly the virus expanded. One of the challenges is that
we were in the midst of the outbreak and then confronted with the
reality that one needs to develop tests. It’s one thing
to develop a test. It’s another to scale it to
the quantities that we’re talking. I mean, we’re talking millions
and millions of tests. Early on, the U.S. focused on using
new tests developed by the CDC that were revealed to be faulty instead
of using tests already established elsewhere. It’s completely unclear to
me why the U.S. screwed up the test approach
because the test was available. There was something that could have been
used and was used by lots of different countries. So it’s
unclear why the U.S. in particular took a different route to
try and develop something of their own. Because everyone else had something
that worked and was using it. Along with shortages of actual tests,
t here have been shortages of materials like swabs and protective gear
that we need to safely perform them. We’ve just chronically had problems
getting tests out there to people. And it’s been a
real bungling of this response. But it wasn’t like that everywhere. The development of a test and the rolling
out that test has not been a disaster in many, many countries. They took the tests that had been developed
and they got it working up in their diagnostic labs and their academic
labs to the level that they needed to use to get Covid-19
under control in their country. There are countries that decided not
to take that route for whatever reason, but that meant that they
lost weeks compared to those countries who brought them in really fast. And what we’re seeing with Covid-19
is that every day counts. On May 7, the head of the National
Institutes of Health said that the U.S. will work with companies to make millions
of accurate and easy to use corona virus tests by the end of
the summer, a timeline that NIH director Francis Collins said was beyond what
most experts think will be possible. Nonetheless, as time passes, testing will
remain critical for knowing not only who is currently infected, but
also who has been previously infected. It’s only when there are not enough
people left to infect that viruses will start to disappear. And so the point,
I guess, is that for this particular virus, that’s probably such a large number
of people that this is going to continue to go on for some time. So even those countries that look like
they are peaking now may well end up seeing more waves of the virus
if there are still more susceptible people around. This antibody tests will
give us critical, it’ll be critical in determining the country’s
approach to reopening markets and safely returning employees
back to work.