As of April 30, over 1 million people have officially recovered from COVID-19. Unofficially, that number is probably much higher. But the road to recovery isn’t always a smooth one. The timeline differs from person to person, but generally, the sicker they are, the longer it takes to get better. Here’s what recovering from COVID-19 looks like, day by day.
MORE CORONAVIRUS COVERAGE:
What Coronavirus Symptoms Look Like, Day By Day
What Could Be The Fastest Way To End The Coronavirus Crisis?
Can You Get The Coronavirus Twice?
——————————————————
#Coronavirus #Recovery #ScienceInsider
Science Insider tells you all you need to know about science: space, medicine, biotech, physiology, and more.
Visit us at: https://www.businessinsider.com
Science Insider on Facebook: https://www.facebook.com/BusinessInsiderScience/
Science Insider on Instagram: https://www.instagram.com/science_insider/
Business Insider on Twitter: https://twitter.com/businessinsider
Tech Insider on Twitter: https://twitter.com/techinsider
Business Insider/Tech Insider on Amazon Prime: http://read.bi/PrimeVideo
——————————————————
What Coronavirus Recovery Looks Like, Day By Day
Most people recover from COVID-19. As of April 30, we’re looking at more than 1
million survivors globally. And if we consider people
who haven’t been tested, that number is probably much higher. But the road to recovery
isn’t always a smooth one. Here’s what it’s like to get better from COVID-19, day by day. Generally, the sicker a person is, the longer it takes to recover, but there’s still a lot we
don’t know about COVID-19. Because it’s not just about how you feel. We have to talk about
transmissibility, too. Mild cases, which are about
80% of all confirmed cases, can run the gamut from
asymptomatic to more serious. Asymptomatic cases are important because even if people
don’t show symptoms, they can still transmit the virus. The CDC estimates that
as many as 25% of people who are infected won’t show symptoms. These people should only break isolation after seven days have passed since their first positive test and no symptoms show up
within that time frame. Mild cases with symptoms
usually don’t require a stay in a hospital and can be managed from home. Recovery can take about two weeks. In that time, fatigue, muscle aches, and chest discomfort should start to ease. If they have a fever, it will most likely settle after a week, though a cough might
linger a little longer. If patients were officially diagnosed with COVID-19 and sent home, the CDC recommends they
meet three criteria before breaking self-isolation: They’ve been fever-free for 72 hours, respiratory symptoms like chest pain or a cough have cleared up, and at least seven days have passed since they saw their first symptoms. Since it’s not fully known how long COVID-19 patients
are contagious for, some experts believe these
current CDC guidelines aren’t conservative enough. Moderate cases are even
tougher to categorize. Some of these will follow a
similar timeline as mild ones, but some might start to look
better after about a week and then suddenly get worse. This could land them in the
hospital for two to three days. Some patients with high
fevers and diarrhea might get dehydrated
and require IV fluids, and since this virus mainly
attacks the respiratory system, a heightened immune response can end up flooding the lungs with fluid. So patients in this category
might need supplemental oxygen for a few days to help
them breathe better, giving the lungs time to
clear up the infection and start working better again. But when this doesn’t work, then we’re looking at severe cases. Symptoms tend to get much
worse around the 10-day mark. A severe case is usually
marked by pneumonia, and recovery time for these patients is around three to six weeks, but pneumonia can sometimes turn into acute respiratory distress
syndrome, or ARDS. That’s when the lungs
are flooded with fluid and the body is severely
deprived of oxygen. ARDS is usually what sends a
COVID-19 patient to the ICU, and the World Health
Organization estimates about 5% of COVID-19
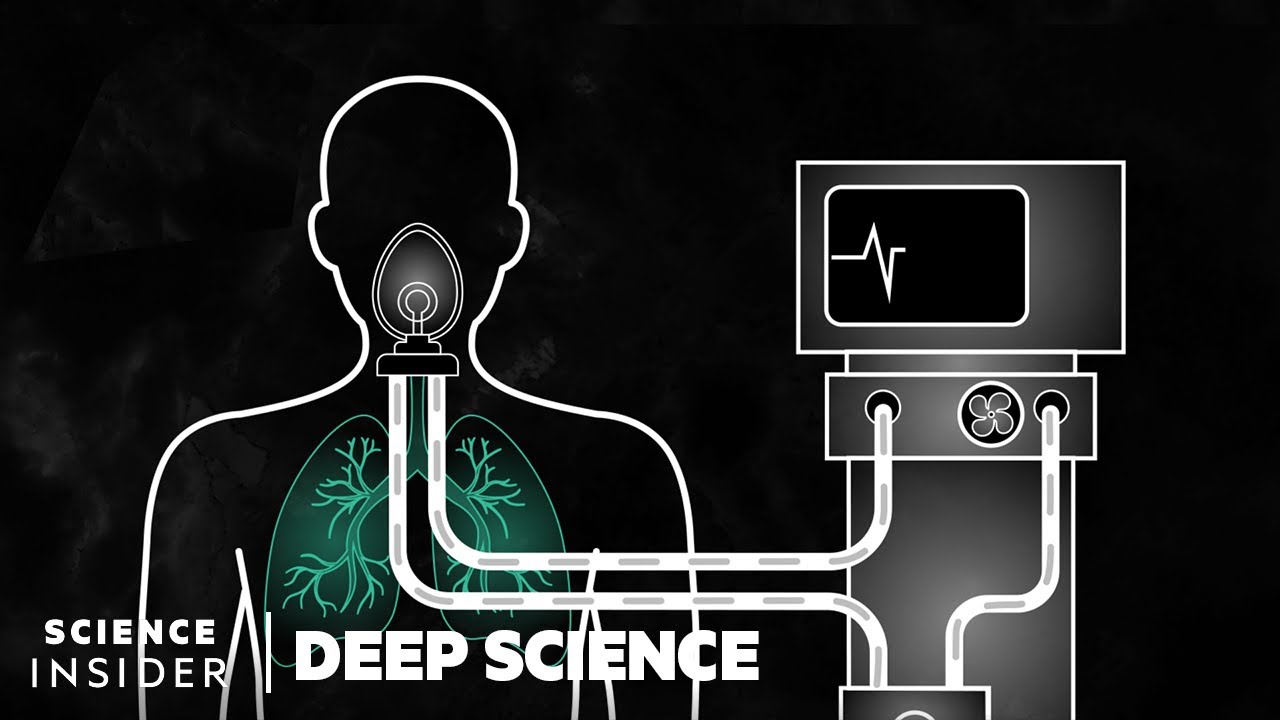
cases will end up there. These are the people who
need to be on ventilators, machines that move air in and out of the lungs for a patient. This provides a greater
supply of oxygen to the lungs while removing carbon dioxide. Some patients may only spend
a couple of weeks ventilated and then a few days recovering in a medical or surgical ward, but ventilation can be an uncomfortable and traumatic process. Patients will need medication
to relieve the discomfort. Many get small doses, but higher ones can
sometimes induce delirium, a change in the brain that can cause mental
or emotional confusion, and it can have a lasting
impact on the recovery process, even potentially causing PTSD, so ventilators are
oftentimes the last resort. A patient is taken off a ventilator after meeting three criteria: They’re able to control their breathing and swallowing on their own; their oxygen levels are high enough that they can be supported
by something less invasive, like a nasal canula; and their lungs can clear carbon dioxide effectively enough not to need assistance. Once off the ventilator, patients usually fall
into one of two camps. Best cases, they’re up and walking. Some can feel a little weak and might have some
weight loss and mild PTSD. They might be able to just take it easy for a week or two to
regain their strength. The worst cases might not
be able to get out of bed. They might be forgetful or confused, probably from delirium, but the physical damage would most likely be seen on the lungs. After severe respiratory
disease and ventilation, many patients will have
pulmonary fibrosis. That could leave the lungs
scarred and less functional. Patients could require rehabilitation, which could mean staying
a couple of months in a skilled nursing facility
before they can go home, and it could take upwards of a year working with psychologists,
speech therapists, and other medical
professionals to work through the effects of a ventilator. So, in the worst cases, after the patient finally
leaves the hospital, it could take up to 18 months before they really feel back to normal. We’re still too early on in this pandemic to know everything about recovery, which is part of the reason the current number of
recovered patients is so low. Many people are still sick,
but will eventually get better. And the more people who recover, the more we’ll learn, and vice versa. For now, the best thing we can do is try to lessen the number of people who get sick in the first place. So, wash your hands, keep
your distance, and be patient.