The management of knee OA primarily focuses on symptom control and functional improvement. Recently, nutritional supplements, particularly collagen-based products, have garnered interest because of their potential role in cartilage metabolism and promising results in previous studies16. Our study evaluated the efficacy of combined UC-II and hydrolysed collagen supplementation in patients with knee OA. Although both intervention and placebo groups demonstrated significant improvements in pain and functional outcomes over the 12-week study period, no significant differences were observed between the groups across all measured parameters, including pain intensity, functional scores, rescue medication consumption, and patient satisfaction.
These findings differ from those of several previous studies that have examined UC-II supplementation alone. Sadigursky et al.17 reported significant improvements in both Western Ontario and McMaster University Arthritis Index (WOMAC) Pain and visual analogue scale (VAS) scores at 30 and 90 d in the UC-II group compared with those in the placebo group. Similarly, Lugo et al.12 observed superior outcomes in the UC-II group across all WOMAC subscales, including significant reductions in pain and VAS scores on day 180.
However, our results aligned more closely with those of Costa et al.,18 who also found no significant differences between the UC-II and placebo groups.
Regarding functional outcomes, our findings contradicted those of several previous studies. We observed no significant improvements in KOOS scores between the groups; however, Sadigursky et al.17 demonstrated significant enhancements in WOMAC function scores and SF-12 physical components by day 90. Similarly, Lugo et al.12 reported superior outcomes across all functional parameters in the UC-II group on day 180.
When comparing our results with those of previous studies on hydrolysed collagen, we found similar disparities. While earlier research by Trč and Bohmová19, Benito-Ruiz et al.,14 and Bruyère et al.20 reported superior pain relief with collagen hydrolysate compared with control interventions, our combined supplementation approach did not yield similar benefits. Notably, Trč and Bohmová19 demonstrated that compared with glucosamine sulphate, enzymatic hydrolysed collagen resulted in significant VAS improvements, while Benito-Ruiz et al.14 observed marked improvements in both VAS and WOMAC scores, particularly among severe OA cases.
The discrepancy between our findings and those of previous studies may be attributed to several factors including supplement formulation variations, dosing regimens, study durations, and patient populations.
Notably, previous trials of individual collagen products such as Lugo et al.12Sadigursky et al.17and Benito-Ruiz et al.14 reported significant improvements in pain and function with intervention durations of 90 days to 6 months. In contrast, our study assessed a combined formulation over a shorter 12-week period. It is possible that the clinical benefits of collagen supplementation, particularly those related to cartilage metabolism and repair, may require longer durations to become detectable. The relatively short timeframe in our study may therefore have limited the ability to observe meaningful differences between groups.
The absence of superior outcomes in the combined supplementation group may suggest a lack of synergistic interaction between UC-II and hydrolysed collagen. These two compounds may even compete for absorption or bioactivity pathways. Additionally, the dosages used in this study (20 mg UC-II and 480 mg hydrolysed collagen) may be suboptimal when administered together. The fixed dosing may not reflect the ideal ratio or threshold needed for synergistic effects. Future studies should explore optimal dosing strategies, timing of administration, and potential pharmacokinetic interactions between these agents to determine whether combined use can offer additive or synergistic clinical benefits.
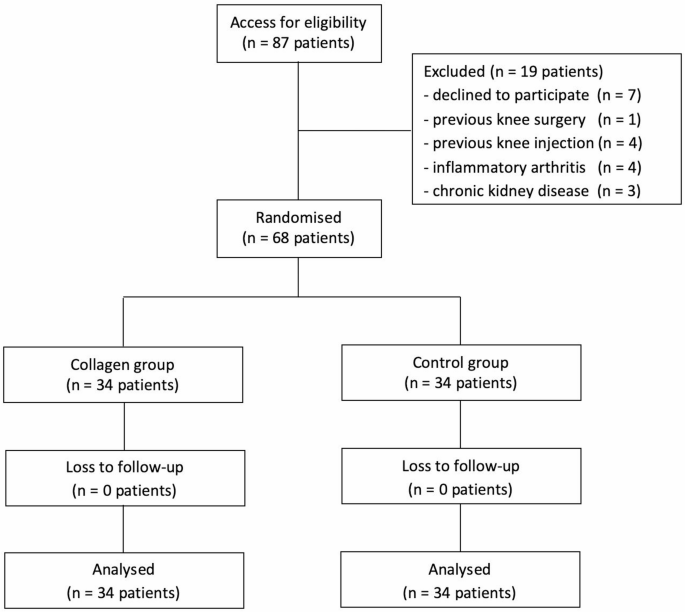
Our study has several limitations. First, the 12-week follow-up period may have been insufficient to detect the long-term effects of collagen supplementation on cartilage metabolism and clinical outcomes, as the biological effects of nutritional interventions often require extended durations to manifest. Second, the relatively small sample size may have resulted in insufficient statistical power to detect small but potentially clinically meaningful effects. A post hoc power analysis using the observed between-group difference in pain reduction (0.08 on the VNRS) and an estimated standard deviation of 2.0 yielded a very small effect size (Cohen’s d = 0.04), corresponding to only 5.3% power with our current sample size (n = 34 per group). Based on conventional estimates for nutraceutical trials, a small-to-moderate effect size (Cohen’s d = 0.3) would require approximately 235 participants per group to achieve 90% power at a 0.05 significance level. Therefore, the null findings should be interpreted cautiously, as the study may have been underpowered to detect subtle benefits. Future research with larger sample sizes is warranted to more definitively assess efficacy.
Third, the study did not include objective biomarkers, imaging data, or pharmacokinetic assessments, which limits our ability to evaluate potential disease-modifying effects or confirm treatment adherence. Future studies should consider incorporating serum or synovial biomarkers, pharmacokinetic analyses, or imaging modalities such as MRI to better understand the biological impact of collagen supplementation and to verify compliance. Additionally, the single-centre recruitment and predominance of moderate knee OA cases (Kellgren–Lawrence grade 2–3) may limit the generalisability of our findings to patients with varying disease severities or from different clinical settings. Although rescue medication consumption was monitored, individual variations in pain threshold and medication usage behaviours could have influenced analgesic patterns. Nonetheless, the randomised double-blind design and comprehensive assessment of both objective and patient-reported outcomes provide robust support for our primary conclusions.