Ever found yourself staring at a grocery shelf, paralyzed by a headline that claims eggs are a superfood one day and a health risk the next? Constant collective whiplash isn’t your fault. Current understanding of what we eat rests on a shaky foundation—a structural “data drought” where high-stakes health advice often stems from little more than memory and guesswork.
We have perfected the tracking of movement and cardiac rhythm through sophisticated digital sensors, yet the intricate metabolic pathways that convert meals into cellular energy remain largely unquantified. Resolving this evidentiary deficit necessitates more than improved mobile applications; it requires a systemic reconstruction of our foundational research infrastructure.
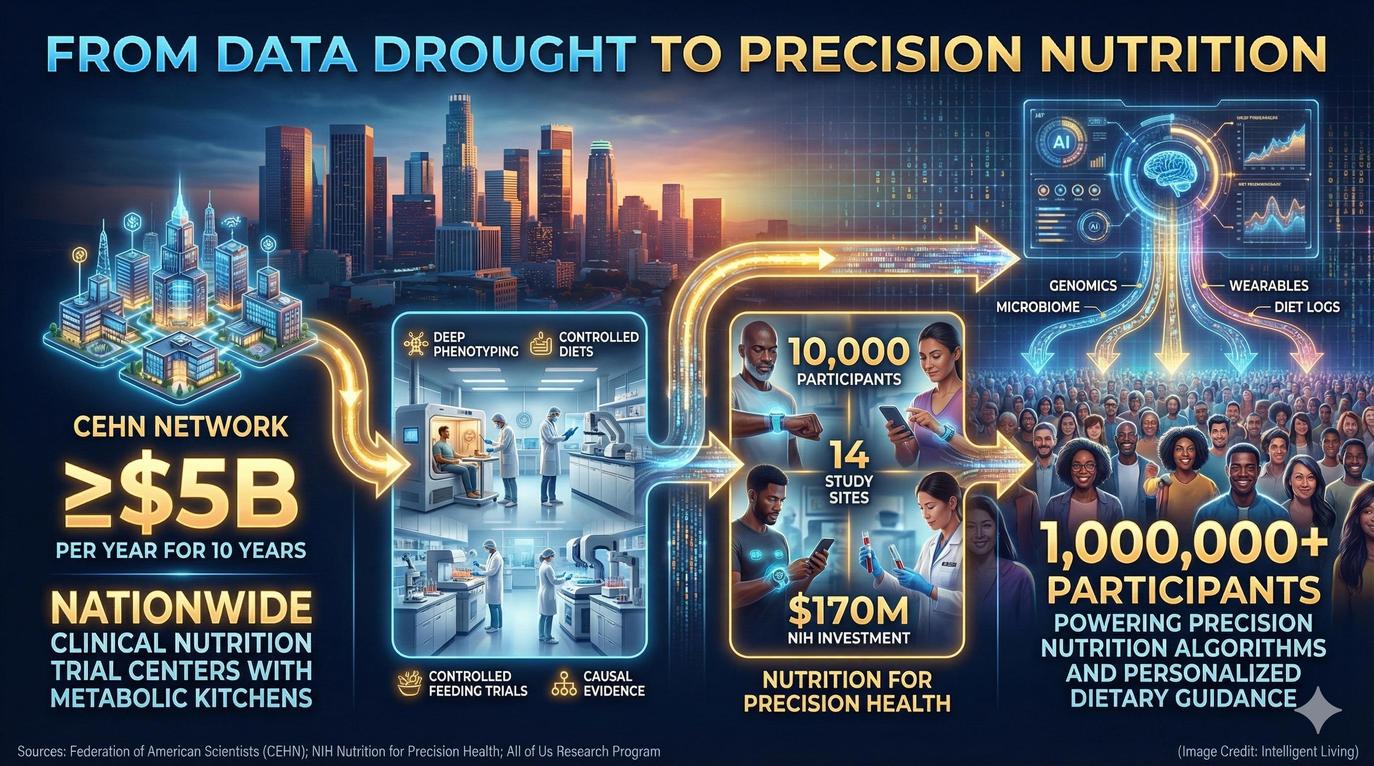
The Federation of American Scientists recently outlined a bold blueprint to replace fragile self-reporting with a network of Centers of Excellence in Human Nutrition (CEHN). Imagine clinical wards where meals are prepared with pharmaceutical precision and metabolic kitchens serve as laboratories for the human body. Specialized clinical methodology transcends simple dietary adjustments, providing the rigorous framework required to definitively validate how specific nutrients interact with unique genomic signatures.
 (Credit: Intelligent Living)
(Credit: Intelligent Living)
Navigating the Evidence Crisis in Modern Nutrition
Bridging the Gap Between Wearables and Clinical Rigor
Merging these heavy-duty research hubs with the digital agility of wearables and AI allows us to finally move past the era of vague correlations. Robust investment promises a shift from population-wide averages to evidence-based interventions that actually work for the individual.
We are standing at the threshold of a nutrition revolution where data isn’t just gathered but verified under the microscope of clinical rigor, transforming “healthy eating” from a guessing game into a precise, personal science.
Critical Factors Behind the Nutrition Research Infrastructure Gap
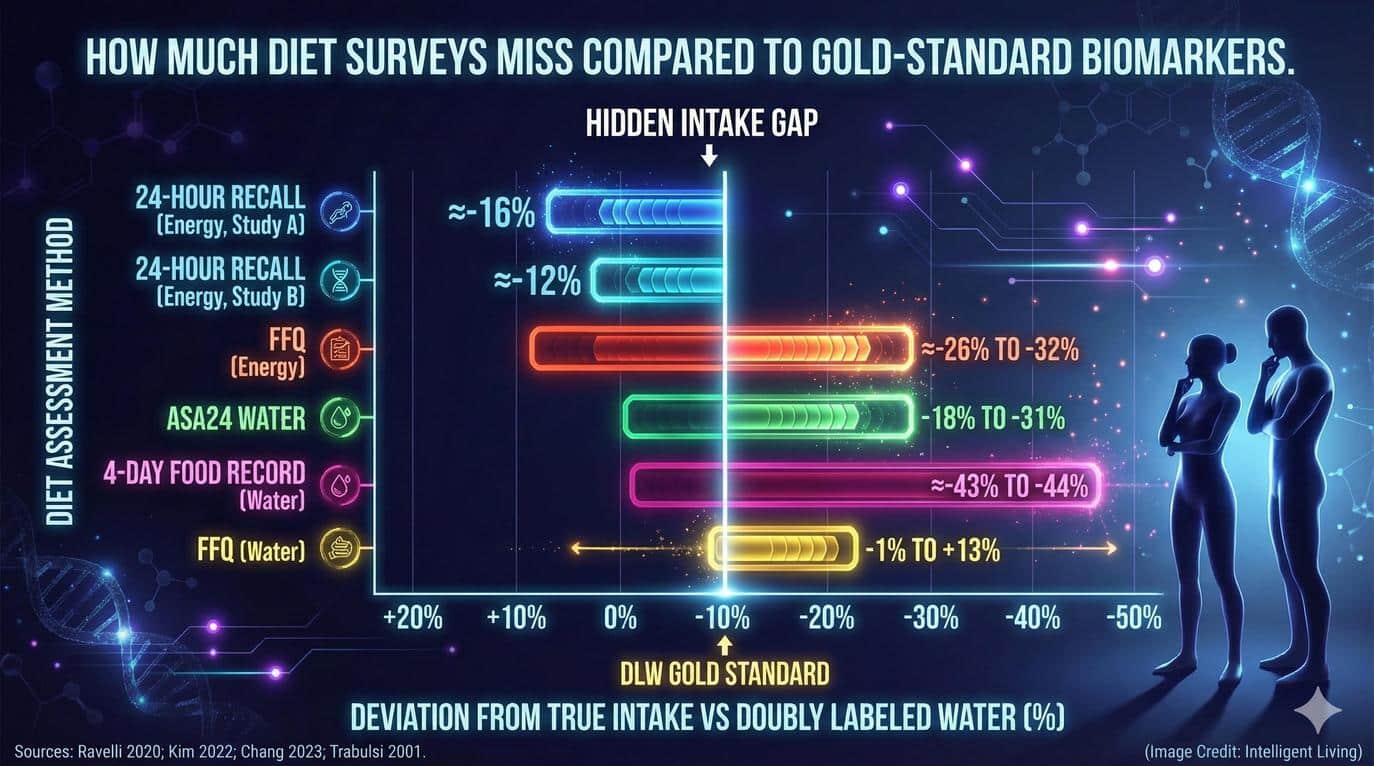
Subjective dietary reporting lacks reliability: Studies show consistent underreporting of calorie intake, particularly among individuals with higher body mass indexes, making it difficult to interpret diet-disease links accurately.
Controlled feeding trials are rare: These trials, which monitor every meal participants eat, are expensive and logistically demanding, leading to a shortage of causal dietary data.
The U.S. lacks research infrastructure: Existing clinical trial centers, such as the NIH’s Clinical and Translational Science Awards program, are not designed for national-scale diet intervention studies.
AI-driven precision nutrition is emerging: Programs like NIH’s Nutrition for Precision Health (NPH) aim to predict individual responses to foods using genetics, microbiome data, and wearable sensors.
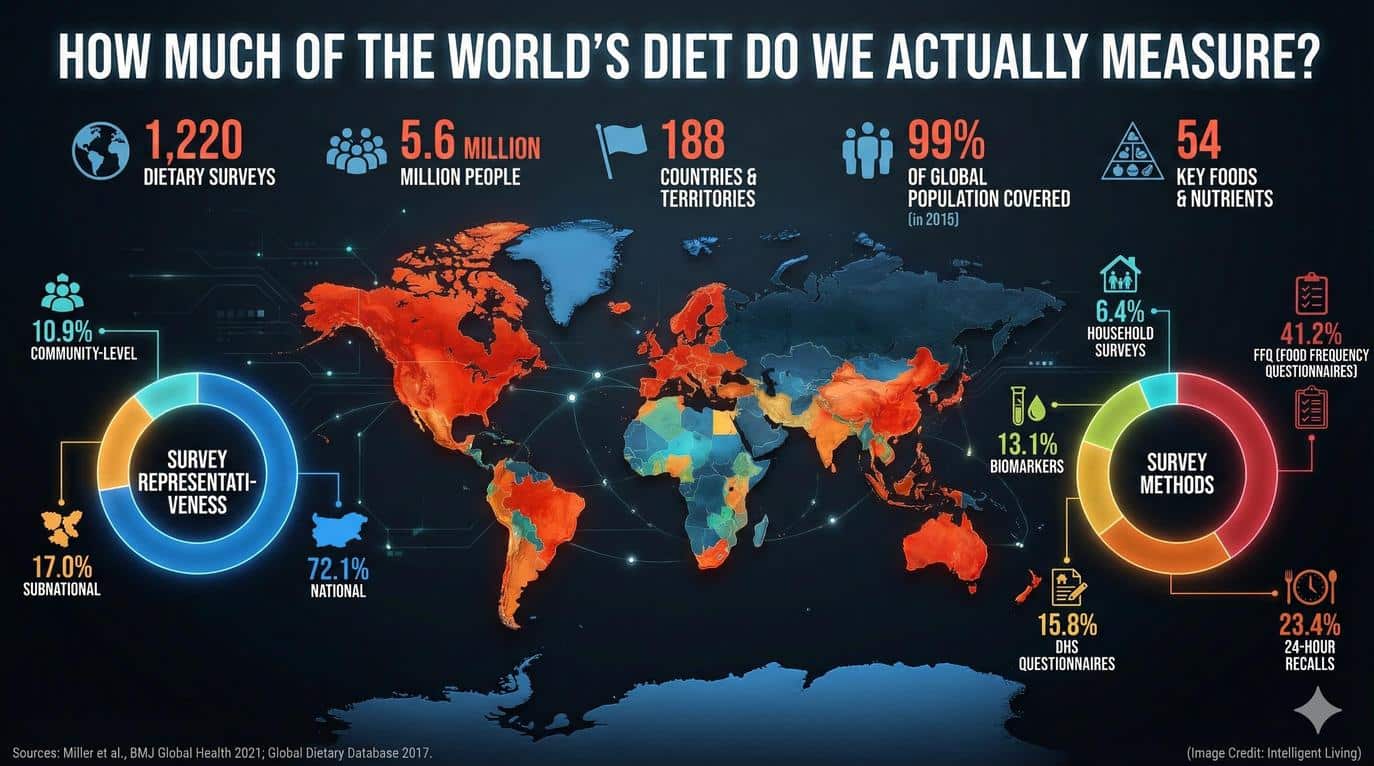
Global nutrition data remains fragmented: Despite projects like the Global Dietary Database, most countries still lack standardized, comparable diet records.
 (Credit: Intelligent Living)
(Credit: Intelligent Living)
Defining the Nutrition Science Data Drought: Beyond Observational Limitations
Rather than a lack of academic interest, a “data drought” represents a deficit in high-quality evidence capable of establishing definitive cause and effect. Much of what we know about diet and disease comes from observational studies, where people report what they eat and researchers look for correlations.
However, these studies often suffer from inaccuracies in self-reporting and confounding variables that make it impossible to determine whether food choices truly drive health outcomes. Inadequate data foundations fuel public skepticism regarding the consistency of nutritional findings. Structural reforms must prioritize the quality of dietary evidence over the mere volume of observational reports.
Peer-reviewed studies investigating self-reported energy intake reveal that participants frequently underestimate caloric consumption, leading to skewed energy balance conclusions. Without direct observation or controlled interventions, researchers can only infer relationships rather than prove them. This weak data foundation contributes to the public perception that nutrition science “always changes its mind.” In reality, it is the data quality, not the scientists, that needs the upgrade.
Why Nutrition Can’t Run “Drug-Grade” Trials by Default
Executing a controlled dietary intervention presents significantly greater complexities than the standardized protocols used in clinical pharmaceutical trials. In a pharmaceutical trial, researchers can easily standardize dosages, placebos, and blinding. With food, these controls are nearly impossible.
Meals necessitate preparation, storage, and delivery under stringently regulated conditions. Participants must then adhere to these assigned diets for extended durations, as inconsequential deviations in participant adherence risk compromising the integrity of longitudinal results.
Financial and Compliance Challenges in Residential Feeding Studies
Significant financial and logistical hurdles also persist, as controlled feeding trials necessitate dedicated kitchens, trained dietitians, and often residential stays to ensure compliance. Without specialized facilities, it’s nearly impossible to measure precisely what participants consume or how their metabolism responds. These logistical hurdles explain why most nutrition data today comes from less rigorous designs. To truly understand how specific foods affect human biology, we need infrastructure built for food science, not retrofitted from drug research.
 (Credit: Intelligent Living)
(Credit: Intelligent Living)
The Infrastructure Gap: What We Lost When Metabolic-Kitchen Capacity Atrophied
In the mid-20th century, the United States had dozens of metabolic research units capable of conducting controlled feeding trials. Dwindling federal funding eventually shuttered dozens of metabolic research units or forced a shift toward competing priorities. Resource scarcity has created an ecosystem where high-quality nutrition experiments are rare and fragmented. These small-scale studies fail to inform national dietary policy, further exacerbating the nutrition science data drought.
Existing federal medical research support systems provide broad clinical funding but lack the specialized infrastructure required for complex dietary interventions. Without this dedicated infrastructure, scientists can’t easily reproduce studies or scale findings across populations.
The discipline shifted toward an overreliance on observational data, leaving a void in precision nutrition trials that could definitively establish biological causation. This gap has left policymakers and the public navigating a flood of conflicting advice based on limited experimental grounding.
The CEHN Proposal: What a Real “Nutrition Trial Network” Would Include
The proposed Centers of Excellence in Human Nutrition (CEHN) aim to fill that gap by rebuilding a nationwide infrastructure for diet research. Modern research hubs require a specialized array of clinical instruments to capture the full complexity of human metabolism. Integrated facilities within the CEHN network would leverage the following assets:
Advanced metabolic kitchens for precise caloric control
Inpatient research wards for continuous participant monitoring
Sophisticated phenotyping tools to record real-time physiological responses
Leveraging Multi-Site Clinical Frameworks for Diverse Populations
Multi-site trials conducted in partnership with community clinics and universities ensure these findings reflect diverse populations and real-world conditions. This collaborative framework allows researchers to scale precision nutrition trials across broad demographic spectrums.
Comprehensive blueprints for rebuilding nutrition research capacity suggest that CEHN centers require an annual investment of approximately $5 billion. That level of investment would enable hundreds of simultaneous controlled feeding studies, dramatically increasing the volume of reliable dietary data. Researchers could directly test the health effects of processed foods, additives, and plant-based diets while incorporating data from wearable sensors and microbiome analyses.
The CEHN model would also integrate with precision nutrition initiatives such as the NIH’s Nutrition for Precision Health program. Together, these efforts could finally move nutrition science toward individualized, evidence-based dietary recommendations backed by rigorous experimentation rather than self-reporting alone.
 (Credit: Intelligent Living)
(Credit: Intelligent Living)
Overhauling Data Collection with Biomarkers and Continuous Physiological Monitoring
Revitalizing nutrition research necessitates a comprehensive transformation of established data acquisition protocols. For decades, the field has relied on self-reported diet surveys—food frequency questionnaires and 24-hour recalls—that depend on memory and honesty. Modern digitized dietary reporting systems have attempted to streamline this process, yet the fundamental constraint of human recall remains unaddressed.
Scientists are increasingly pivoting toward biomarkers to bypass the limitations of human memory. These measurable substances in blood, urine, or tissues provide an objective reflection of true dietary intake. Clinical precision improves when specific markers reveal exact consumption patterns.
Integrating Digital Health Platforms with Objective Biomarker Analysis
Certain fatty acids can confirm fish intake, while urinary sodium levels provide an accurate approximation of salt consumption. Combining these biomarkers with digital tools like wearables and smart food logs provides a clearer picture of real dietary behavior. Objective findings allow practitioners to move beyond traditional labs into sophisticated metabolic care platforms that provide real-time biomarker dashboards.
Wearable devices, from continuous glucose monitors to smartwatches, are bridging the gap between subjective reporting and physiological reality through advanced sensor ecosystems. Continuous monitoring is bridging the gap between subjective memory and verifiable physiological reality through advanced sensor ecosystems. They offer real-time insights into metabolism, activity, and sleep—all factors that influence nutrition outcomes. However, wearables are not yet universal research tools. Their data needs to be standardized, validated, and integrated with established methods to ensure consistency across studies.
Systemic integration of controlled feeding studies, digitized records, objective biomarker analysis, and continuous physiological monitoring will create a unified evidence framework. This integration is essential to produce the kind of robust, reproducible data that modern nutrition science demands.
 (Credit: Intelligent Living)
(Credit: Intelligent Living)
Scaling Precision Nutrition Trials through Robust Foundational Data
Precision nutrition promises a future where dietary recommendations are tailored to each individual’s unique biology. Large-scale precision health studies are currently analyzing multi-omic data from thousands of participants to refine dietary algorithms. The goal is to develop algorithms capable of predicting how specific foods affect each person’s health.
However, precision nutrition will only work if it’s built on reliable, high-quality input data. Algorithms trained on biased or incomplete datasets risk amplifying the very inaccuracies they aim to correct. This is why the CEHN proposal and measurement reforms are so critical—they provide the foundational data infrastructure that precision nutrition models depend on.
When combined, these initiatives could shift nutrition science from general guidelines to personalized, evidence-based interventions. Clinical practice is evolving toward a model where practitioners recommend specific nutrients based on individualized gut microbiomes, genomic profiles, and dynamic metabolic responses. Evidence-based interventions will likely manifest as adaptive dietary technologies capable of modifying coaching protocols based on immediate metabolic feedback.
Future dietary strategies will integrate microbiome-targeted nutrient optimization to tailor intake according to individual gut flora. Imagine a future where a dietitian can recommend foods based not just on population averages but on your personal gut microbiome, genetic profile, and real-time metabolic responses. That future begins with better inputs today.
The Global Dimension: Why Diet Data Is Hard to Compare Across Countries
Nutrition science is not just a national issue; it is a global one. Despite increasing awareness of diet-related diseases, many nations still lack the infrastructure to collect and compare dietary data consistently. Collaborative efforts to aggregate international dietary surveys have made progress in 180 countries, yet significant geographic data gaps persist. These gaps reflect broader national food security challenges where few countries can independently sustain the nutritional requirements of their populations.
Global comparisons suffer from a lack of standardized survey methods, portion sizes, and nutrient databases. Regional definitions of a “serving” for staples like vegetables or grains differ significantly, complicating international data synthesis. Limited resources in developing nations often prevent the implementation of national nutrition surveillance programs. This financial barrier leads to chronic underrepresentation in global datasets, leaving critical gaps in our understanding of worldwide health trends.
Standardizing methods through international collaborations can help fill these gaps. Harmonization is possible, but it requires shared data policies, compatible technologies, and long-term funding. Improving global comparability is not just about fairness; it is about ensuring that nutrition policies worldwide are informed by complete and accurate evidence.
 (Credit: Intelligent Living)
(Credit: Intelligent Living)
Restoring Public Confidence and Informing National Dietary Policy
Establishing a robust evidence base benefits researchers while simultaneously restoring public confidence in dietary science. When studies use precise methods and transparent data, dietary guidelines become more credible and less prone to controversy. This clarity can improve how governments craft policies, how companies design healthier foods, and how individuals make choices at the grocery store.
Robust data pipelines empower policymakers to transition from reactive guidelines to proactive health strategies. Verified evidence from metabolic research centers could directly influence high-impact public health initiatives, including:
National sodium reduction mandates based on clinical safety data
Modernized food labeling laws that reflect true nutrient density
Targeted dietary interventions for vulnerable populations
Clinical clarity ensures that national health frameworks are built on a foundation of biological fact rather than observational theory. Verified evidence facilitates informed choices regarding maternal nutrition and epigenetic health, ensuring that dietary decisions positively influence children’s long-term developmental trajectories. Clear, consistent data would also reduce the “whiplash effect” of contradictory headlines that currently fuel skepticism about nutrition research.
In the long term, a transparent, well-funded nutrition evidence ecosystem has the potential to reshape not only public health but also the global food economy. Reliable data builds accountability, and accountability builds trust.
Closing the Gap Between Dietary Guesswork and Proven Biology
Forging a path toward scientific rigor in nutrition necessitates a fundamental pivot from observational anecdotes to sophisticated data infrastructure. When we prioritize the construction of CEHN facilities and modernize our measurement tools, we aren’t just funding labs; we’re investing in the credibility of public health itself. Radical evolution transforms a historically fragmented field into a powerhouse of actionable, individualized insights. The resulting clarity will ripple through every level of society, from the way governments draft national policy to the specific choices a parent makes for their child’s lunchbox.
As the lines between infrastructure, wearable technology, and human behavior data finally blur, the era of nutritional guesswork will inevitably fade. We are moving toward a globally connected ecosystem where diet advice is not only consistent but also scientifically unshakable. The payoff for this persistence is a future where your dinner plate is informed by verifiable, personal data—ensuring that every bite supports a lifetime of optimal health and metabolic resilience.
 (Credit: Intelligent Living)
(Credit: Intelligent Living)
Essential Insights on Nutrition Data and Precision Research
Why do modern nutrition studies often yield conflicting results?
Subjective reporting relies on fallible human memory, which introduces significant bias and error. Without the clinical rigor of controlled experiments, researchers struggle to separate true cause-and-effect from mere coincidence.
What makes controlled feeding trials the gold standard for evidence?
These trials remove variables by providing every meal to participants under strict supervision. This clinical environment allows scientists to measure exact metabolic responses, ensuring the data is both reproducible and causal.
Can wearable health technology replace traditional clinical studies?
Wearables offer brilliant real-time snapshots of our physiology, but they function best as part of a larger team. They must be validated against clinical biomarkers and controlled feeding data to provide a complete picture of health.
How does precision nutrition differ from standard dietary guidelines?
Standard guidelines are built for the “average” person, but precision nutrition looks at your unique genetic and microbiome profile. It uses advanced algorithms to predict exactly how your specific body will react to different foods.
What is the primary goal of the CEHN infrastructure proposal?
The CEHN initiative aims to build a nationwide network of metabolic kitchens and research wards. This infrastructure will generate the high-quality, “drug-grade” data needed to restore public trust in nutrition science.








