Smith, J. P., Thompson, J. F. & Ellwood, D. A. Hospital system costs of artificial infant feeding: estimates for the Australian capital territory. Aust N Z. J. Public. Health. 26, 543–551 (2002).
World Health Organization. Global strategy for infant and young child feeding. World Health Organ. 1–5 (2001).
American Academy of Pediatrics. Breastfeeding and the use of human milk. Pediatrics 115, 496–506 (2005).
Grummer-Strawn, L. M. & Mei, Z. Does breastfeeding protect against pediatric overweight? Analysis of longitudinal data from the centers for disease control and prevention pediatric nutrition surveillance system. Pediatrics 113, e81–e86 (2004).
Quinn, P. J. et al. The effect of breastfeeding on child development at 5 years: a cohort study. J. Paediatr. Child. Health. 37, 465–469 (2001).
Oddy, W. H., De Klerk, N. H., Sly, P. D. & Holt, P. G. The effects of respiratory infections, atopy, and breastfeeding on childhood asthma. Eur. Respir J. 19, 899–905 (2002).
Bachrach, V. R. G., Schwarz, E. & Bachrach, L. R. Breastfeeding and the risk of hospitalization for respiratory disease in infancy: a meta-analysis. Arch. Pediatr. Adolesc. Med. 157, 237–243 (2003).
Suliman, O. et al. The effect of weaning practices on the nutritional and health status of Saudi preschool children. Cureus 15, e47273 (2023).
White, J. M. Weaning: what influences the timing?. Community Pract. 82, 34–37 (2009).
Tarrant, M. et al. Breastfeeding and weaning practices among Hong Kong mothers: a prospective study. BMC Pregnancy Childbirth. 10, 1–12 (2010).
Ajmal, S., Ajmal, L., Ajmal, M. & Nawaz, G. Association of malnutrition with weaning practices among infants in Pakistan. Cureus 14, e31018 (2022).
Amr, M. & Farid, A. Impact of cow, buffalo, goat or camel milk consumption on oxidative stress, inflammation and immune response post weaning time. Sci. Rep. 14, 9967 (2024).
Mustafa, A. B. et al. Impact of early weaning on constituents and nutritional values of camel milk in modern system. Open. Vet. J. 10, 232–238 (2020).
Liu, Y. & Zhang, F. Comparison of whole goat milk and its major fractions regarding the modulation of gut microbiota. J. Sci. Food Agric. 102, 3618–3627 (2022).
Ayoub, M. A. et al. Invited review: camel milk–derived bioactive peptides and diabetes—Molecular view and perspectives. J. Dairy. Sci. 107, 649–668 (2024).
Liu, Y., Cai, J. & Zhang, F. Functional comparison of breast milk, cow milk and goat milk based on changes in the intestinal flora of mice. LWT – Food Sci. Technol. 150, 111976 (2021).
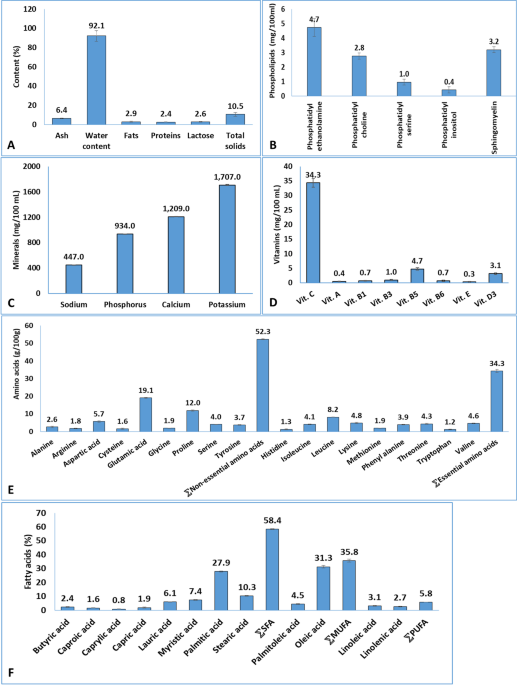
Bakry, I. A. et al. How does camel milk fat profile compare with that of human milk fat to serve as a substitute for human milk? Int. Dairy. J. 146, 105738 (2023).
Al-Awadi, F. M. & Srikumar, T. S. Trace elements and their distribution in protein fractions of camel milk in comparison to other commonly consumed milks. J. Dairy. Res. 68, 463–469 (2001).
Ismail, L. C. et al. Camel milk consumption patterns and perceptions in the UAE: A cross-sectional study. J. Nutr. Sci. 11, e59 (2022).
Mirmiran, P., Ejtahed, H. S., Angoorani, P., Eslami, F. & Azizi, F. Camel milk has beneficial effects on diabetes mellitus: A systematic review. Int. J. Endocrinol. Metab. 15, e42176 (2017).
Ayoub, M. A., Palakkott, A. R., Ashraf, A. & Iratni, R. The molecular basis of the anti-diabetic properties of camel milk. Diabetes Res. Clin. Pract. 146, 305–312 (2018).
Amr, M., Mohie-Eldinn, M. & Farid, A. Evaluation of buffalo, cow, goat and camel milk consumption on multiple health outcomes in male and female Sprague Dawley rats. Int. Dairy. J. 146, 105760 (2023).
Agoston, D. V. How to translate time? The Temporal aspect of human and rodent biology. Front. Neurol. 8, 92 (2017).
Almasri, R. S., Bedir, A. S., Ranneh, Y. K., El-Tarabily, K. A. & Al Raish, S. M. Benefits of camel milk over cow and goat milk for infant and adult health in fighting chronic diseases: A review. Nutrients 16, 3848 (2024).
Riley, L. K., Rupert, J. & Boucher, O. Nutrition in toddlers. Am. Fam Physician. 98, 227–233 (2018).
Liu, Z., Moate, P. & Rochfort, S. A simplified protocol for fatty acid profiling of milk fat without lipid extraction. Int. Dairy. J. 90, 68–71 (2019).
Kamal, A. M., Salama, O. A. & El-Saied, K. M. Changes in amino acids profile of camel milk protein during the early lactation. Int. J. Dairy. Sci. 2, 226–234 (2007).
Antakli, S., Sarkees, N. & Sarraf, T. Determination of water-soluble vitamins B1, B2, B3, B6, B9, B12 and C on C18 column with particle size 3 µM in some manufactured food products by HPLC with UV-DAD/FLD detection. Int. J. Pharm. Pharm. Sci. 7, 219–224 (2015).
Guneser, O. & Yuceer, Y. K. Effect of ultraviolet light on water- and fat-soluble vitamins in cow and goat milk. J. Dairy. Sci. 95, 6230–6241 (2012).
Wei, W. et al. Phospholipid composition and fat globule structure I: comparison of human milk fat from different gestational ages, lactation stages, and infant formulas. J. Agric. Food Chem. 67, 13922–13928 (2019).
World Health Organization Multicentre Growth Reference Study Group. WHO Child Growth Standards: Length/height-for-age, weight-for-age, weight-for-length, weight-for-height: Methods and Development (World Health Organization, 2006).
World Health Organization. Guideline: Updates on the Management of Severe Acute Malnutrition in Infants and Children (World Health Organization, 2013).
Van Loveren, H., Verlaan, A. P. J. & Vos, J. G. An enzyme-linked immunosorbent assay of anti-sheep red blood cell antibodies of the classes M, G, and A in the rat. Int. J. Immunopharmacol. 13, 689–695 (1991).
Bourguignon, C., Dupuy, A. M., Coste, T., Michel, F. & Cristol, J. P. Evaluation of NM-BAPTA method for plasma total calcium measurement on Cobas 8000®. Clin. Biochem. 47, 636–639 (2014).
Costa, M. B., Lanna, C. M. M. & Braga, M. H. Assessment of asymptomatic hypercalcemia in outpatients. J. Bras. Patol. Med. Lab. 44, 329–335 (2008).
Arain, M. A. et al. Nutritional significance and promising therapeutic/medicinal application of camel milk as a functional food in human and animals: a comprehensive review. Animal Biotechnol. 34 (6), 1988–2005 (2023).
Arain, M. A. et al. Exploring the anti-diabetic properties of camel milk: effects on blood glucose, antioxidant defense, and organ histo-morphological features in rabbits. J. Mol. Histol. 56 (2), 92 (2025).
Muthukumaran, M. S., Mudgil, P., Baba, W. N., Ayoub, M. A. & Maqsood, S. A comprehensive review on health benefits, nutritional composition and processed products of camel milk. Food Rev. Int. 39, 3080–3106 (2023).
Mohammaddin, A. et al. Effects of camel milk in dyslipidaemia: A randomized clinical trial. Int. Dairy. J. 84, 79–84 (2018).
Arain, M. A., Khaskheli, G. B., Barham, G. S. & Marghazani, I. B. Lactoferrin’s role in modulating NF-κB pathway to alleviate diabetes-associated inflammation: A novel in-silico study. Heliyon 10 (14), e34051 (2024).
Ho, T. M., Zou, Z. & Bansal, N. Camel milk: A review of its nutritional value, heat stability, and potential food products. Food Res. Int. 153, 110870 (2022).
Seifu, E. Recent advances on camel milk: nutritional and health benefits and processing implications—A review. AIMS Agric. Food. 7, 777–804 (2022).
Li, R. R. et al. Protein profile of whole camel milk resulting from commercial thermal treatment. LWT – Food Sci. Technol. 134, 110256 (2020).
Nayik, G. A. et al. Nutritional profile, processing and potential products: A comparative review of goat milk. Dairy 3, 622–647 (2022).
Medhammar, E. et al. Composition of milk from minor dairy animals and Buffalo breeds: a biodiversity perspective. J. Sci. Food Agric. 92, 445–474 (2012).
Zhao, L., Zhang, J., Ge, W. & Wang, J. Comparative lipidomics analysis of human and ruminant milk reveals variation in composition and structural characteristics. J. Agric. Food Chem. 70, 8994–9006 (2022).
Seyiti, S., Kelimu, A. & Yusufu, G. Bactrian camel milk: chemical Composition, Bioactivities, processing Techniques, and economic potential in China. Molecules 29, 4680 (2024).
Zou, X. et al. Lipid composition analysis of milk fats from different mammalian species: potential for use as human milk fat substitutes. J. Agric. Food Chem. 61, 7070–7080 (2013).
Gao, D., Mu, Q., Liu, L. & Guo, J. Determination and comparison on protein and amino acids profile of four kinds of livestock milk in inner Mongolian. Food Sci. 42, 267–272 (2017).
Bakry, I. A. et al. Comparative characterisation of fat fractions extracted from Egyptian and Chinese camel milk. Int. Dairy. J. 105, 104691 (2020).
Teng, F., Wang, P., Yang, L., Ma, Y. & Day, L. Quantification of fatty acids in human, cow, buffalo, goat, yak, and camel milk using an improved one-step GC-FID method. Food Anal. Methods. 10, 2881–2889 (2019).
United States Department of Agriculture. Dietary Guidelines for Americans 2020–2025 (USDA Center for Nutrition Policy and Promotion, 2020).
Williams, K. M. Update on bone health in pediatric chronic disease. Endocrinol. Metab. Clin. North. Am. 45, 433–441 (2016).
Jiao, L. et al. Estrogen and calcium handling proteins: new discoveries and mechanisms in cardiovascular diseases. Am. J. Physiol. -Heart Circ. Physiol. 318, H820–H829 (2020).
Soldin, O. P., Hoffman, E. G., Waring, M. A. & Soldin, S. J. Pediatric reference intervals for FSH, LH, estradiol, T3, free T3, cortisol, and growth hormone on the DPC IMMULITE 1000. Clin. Chim. Acta. 355, 205–210 (2005).
Djakpo, D. K., Wang, Z. Q. & Shrestha, M. The significance of transaminase ratio (AST/ALT) in acute myocardial infarction. Arch. Med. Sci. Atheroscler Dis. 5, 279–283 (2020).
Kashani, K., Rosner, M. H. & Ostermann, M. Creatinine: from physiology to clinical application. Eur. J. Intern. Med. 72, 9–14 (2020).
Haines, R. W. et al. Elevated urea-to-creatinine ratio provides a biochemical signature of muscle catabolism and persistent critical illness after major trauma. Intensive Care Med. 45, 1718–1731 (2019).
Griffin, J. W. & Bradshaw, P. C. Effects of a high-protein diet and liver disease in an in Silico model of human ammonia metabolism. Theor. Biol. Med. Model. 16, 1–14 (2019).
Parhofer, K. G. & Laufs, U. Lipid profile and lipoprotein (a) testing. Dtsch. Ärztebl Int. 120, 582 (2023).
Holven, K. B. & van Lennep, J. R. Sex differences in lipids: a life course approach. Atherosclerosis 384, 117270 (2023).
Moghbeli, M. et al. Cytokines and the immune response in obesity-related disorders. Adv. Clin. Chem. 101, 135–168 (2021).
Bouman, A., Heineman, M. J. & Faas, M. M. Sex hormones and the immune response in humans. Hum. Reprod. Update. 11, 411–423 (2005).
Cunningham, M. & Gilkeson, G. Estrogen receptors in immunity and autoimmunity. Clin. Rev. Allergy Immunol. 40, 66–73 (2011).
Kovats, S. Estrogen receptors regulate innate immune cells and signaling pathways. Cell. Immunol. 294, 63–69 (2015).
Hewagama, A., Patel, D., Yarlagadda, S., Strickland, F. M. & Richardson, B. C. Stronger inflammatory/cytotoxic T-cell response in women identified by microarray analysis. Genes Immun. 10 (5), 509–516 (2009).
Grimaldi, C. M., Cleary, J., Dagtas, A. S., Moussai, D. & Diamond, B. Estrogen alters thresholds for B cell apoptosis and activation. J. Clin. Invest. 109, 1625–1633 (2002).
Pauklin, S., Sernández, I. V., Bachmann, G., Ramiro, A. R. & Petersen-Mahrt, S. K. Estrogen directly activates AID transcription and function. J. Exp. Med. 206, 99–111 (2009).
Fink, A. L., Engle, K., Ursin, R. L., Tang, W. Y. & Klein, S. L. Biological sex affects vaccine efficacy and protection against influenza in mice. Proc. Natl. Acad. Sci. U.S.A. 115, 12477–12482 (2015).
García-Durán, M. et al. López-Farré, A. Estrogen stimulates neuronal nitric oxide synthase protein expression in human neutrophils. Circ. Res. 85, 1020–1026 (1999).
Marriott, I., Bost, K. L. & Huet-Hudson, Y. M. Sexual dimorphism in expression of receptors for bacterial lipopolysaccharides in murine macrophages: a possible mechanism for gender-based differences in endotoxic shock susceptibility. J. Reprod. Immunol. 71, 12–27 (2006).
Giefing-Kröll, C., Berger, P., Lepperdinger, G. & Grubeck-Loebenstein, B. How sex and age affect immune responses, susceptibility to infections, and response to vaccination. Aging Cell. 14, 309–321 (2015).
Klein, S. L. & Flanagan, K. L. Sex differences in immune responses. Nat. Rev. Immunol. 16, 626–638 (2016).
Libert, C., Dejager, L. & Pinheiro, I. The X chromosome in immune functions: when a chromosome makes the difference. Nat. Rev. Immunol. 10, 594–604 (2010).
Whitacre, C. C. Sex differences in autoimmune disease. Nat. Immunol. 2, 777–780 (2001).
Martínez, Y. et al. The role of methionine on metabolism, oxidative stress, and diseases. Amino Acids. 49, 2091–2098 (2017).
Carr, A. C. & Maggini, S. Vitamin C and immune function. Nutrients 9, 1211 (2017).
Radzikowska, U. et al. The influence of dietary fatty acids on immune responses. Nutrients 11, 2990 (2019).
Küllenberg, D., Taylor, L. A., Schneider, M. & Massing, U. Health effects of dietary phospholipids. Lipids Health Dis. 11, 1–16 (2012).
O’Donnell, V. B., Rossjohn, J. & Wakelam, M. J. Phospholipid signaling in innate immune cells. J. Clin. Invest. 128, 2670–2679 (2019).
Kandeel, M., Morsy, M. A., Khodair, A., Alhojaily, S. & K. M. & Meta-analysis of the efficacy of camel milk consumption for improving autism symptoms in children in randomized clinical trials. Open. Vet. J. 14, 2441–2452 (2024).
Mebius, R. E. & Kraal, G. Structure and function of the spleen. Nat. Rev. Immunol. 5, 606–616 (2005).
Bronte, V. & Pittet, M. J. The spleen in local and systemic regulation of immunity. Immunity 39, 806–818 (2013).
Rouse, B. T. & Sehrawat, S. Immunity and immunopathology to viruses: what decides the outcome? Nat. Rev. Immunol. 10, 514–526 (2010).