Researchers at the University of Pittsburgh School of Medicine have developed a new approach for tackling insulin resistance and type 2 diabetes by protecting beneficial immune cells in fat tissue.
Scientists at the University of Pittsburgh School of Medicine have identified a new way in which the body may combat insulin resistance and type 2 diabetes, by enhancing a specialised group of beneficial immune cells found in fat tissue.
It is hoped that these preclinical findings could help the development of a new medication aimed at treating and potentially preventing type 2 diabetes. Researchers suggest such a treatment could one day replace or complement GLP-1 weight maintenance drugs, which can lose effectiveness over time.
A growing public health challenge
“One-third of our population is obese or overweight – over the next decade or so, obesity will drive increasing rates of many chronic diseases, including diabetes,” said Dr Partha Dutta, Professor of Cardiology and Director of the Center for Cardiovascular Inflammation in Pitt’s Department of Medicine. “Our discovery could be the key to reversing insulin resistance and curing type 2 diabetes.”
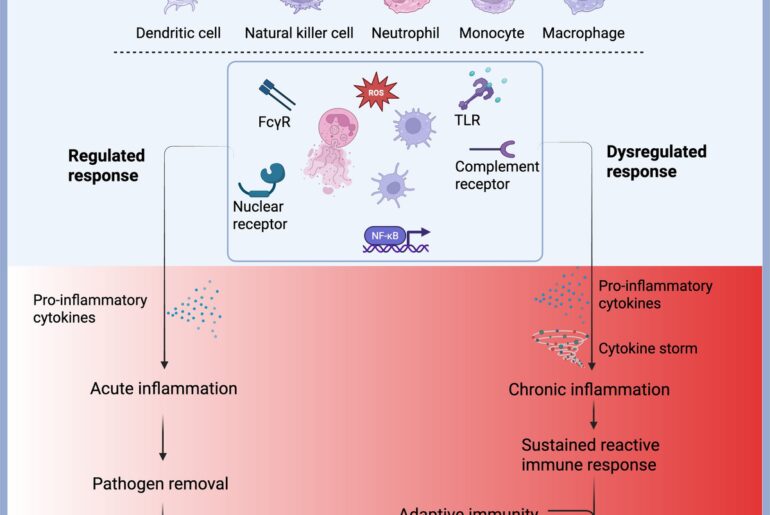
Type 2 diabetes is closely linked to excess body fat, particularly fat that accumulates around abdominal organs. This visceral fat produces inflammatory immune signals that are known to trigger insulin resistance, a condition where the body becomes less responsive to insulin, the hormone responsible for regulating blood sugar.
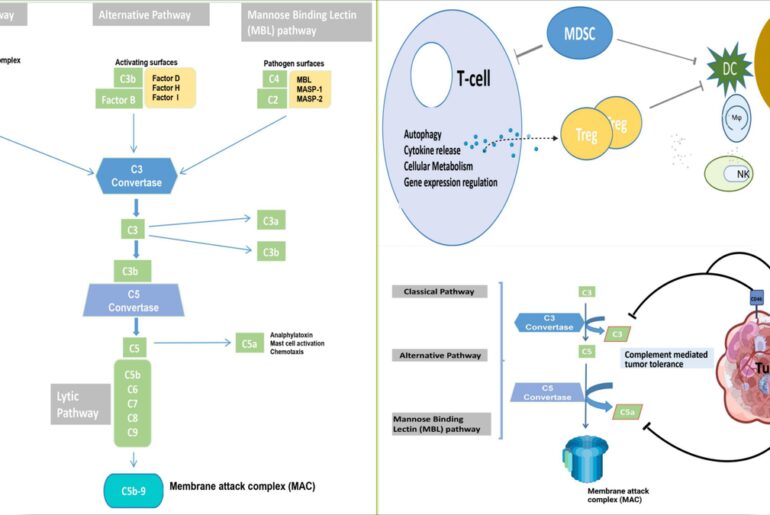
Professor Dutta and researchers at Pitt’s Vascular Medicine Institute set out to better understand the immune processes underlying this link, conducting research in both mice and human tissue.
The role of ‘good’ immune cells
“What we found is that there is a subset of immune cells in our fat tissue that are actually helpful,” said Dutta. “Although they’re immune cells, they’re not inflammatory – rather, they actually suppress the inflammation that causes insulin resistance.”
These beneficial immune cells, known as resident macrophages, are key in maintaining tissue health. They clear away dead cells, fight infection and help preserve normal function within fat tissue.
A protein called SerpinB2 is essential for the survival of resident macrophages. However, when excessive visceral fat builds up, as occurs in people who are overweight or obese, inflammation rises sharply and levels of SerpinB2 fall. As a result, resident macrophages begin to die off.
Without enough of these protective cells, fat tissue can expand unchecked and become highly inflamed. Over time, this heightened inflammatory state interferes with the body’s ability to respond to insulin, eventually leading to the development of type 2 diabetes.
From laboratory findings to future treatments
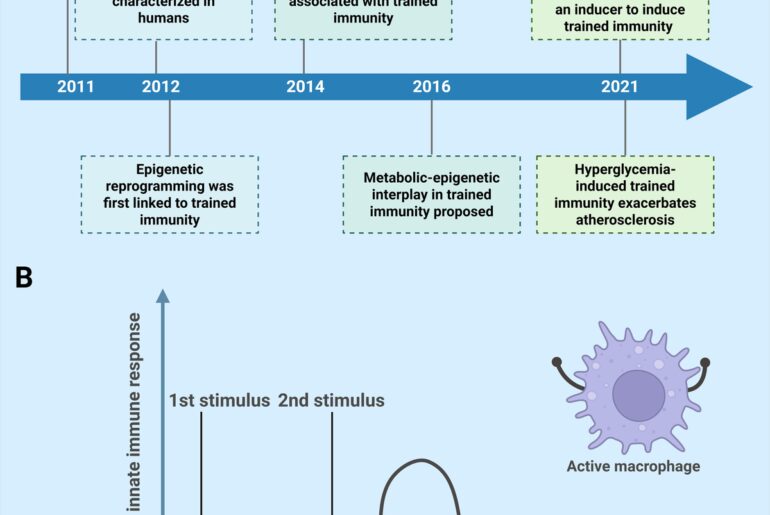
In experiments involving overweight mice with insulin resistance, researchers found that administering antioxidant supplements boosted levels of resident macrophages and improved the animals’ sensitivity to insulin.
The team is now working to translate these findings into human treatments. Their focus is on identifying a small molecule capable of increasing SerpinB2 levels, which could then be developed into a medication for clinical trials. This kind of drug would aim to protect resident macrophages, preventing the cycle of fat accumulation and inflammation that drives type 2 diabetes.
Researchers also believe the approach may benefit individuals who already have the condition, particularly when used alongside GLP-1 weight maintenance therapies.
“Studies are showing that people who have been on GLP-1 medications for a long time develop ‘GLP-1 resistance’ and they plateau,” said Dutta. “Our goal is to develop a drug that will stop and reverse the process that leads to bad fat accumulation and insulin-resistance by protecting and boosting the good immune cells that keep fat tissues healthy.”
Related topics
Animal Models, Disease Research, Drug Development, Drug Discovery, Drug Targets, Immunology, In Vivo, Molecular Targets, Obesity, Pharmacology, Research & Development, Small Molecules, Targets, Therapeutics, Translational Science