NEW YORK, Feb. 18, 2026 /PRNewswire/ — A protein made by stressed cancer cells helps lung and pancreatic tumors evade the immune system, a new study shows.
 (PRNewsfoto/NYU Langone Health) (PRNewsfoto/NYU Langone Health)
(PRNewsfoto/NYU Langone Health) (PRNewsfoto/NYU Langone Health)
Led by researchers from NYU Langone Health, the work found that new drugs designed to block the action of a protein called lipocalin 2 (LCN2) slowed cancer growth in mice by enabling the immune system to target tumor cells. The drugs made aggressive cancers more vulnerable to immunotherapies, which help the immune system attack cancer cells.
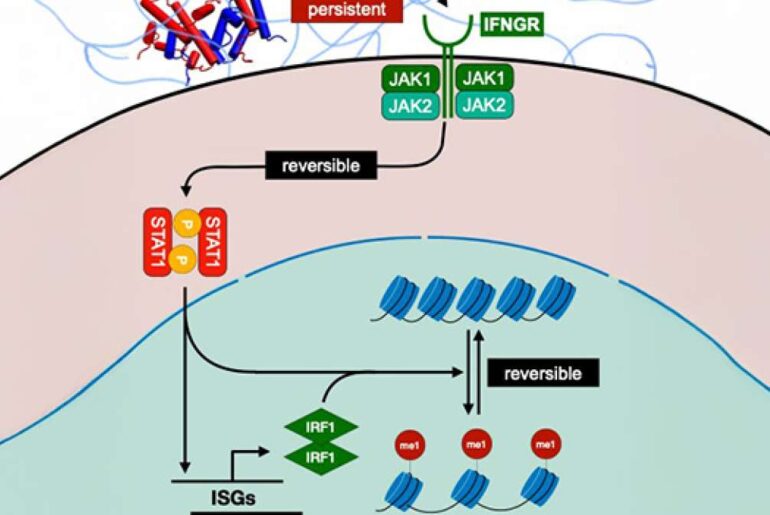
Publishing online February 18 in the journal Nature, the study involved a cellular survival pathway called the integrated stress response (ISR), which cells use to endure stressful conditions, such as a lack of nutrients. Cancer cells, with their abnormal, aggressive growth, face a continual threat of starvation, are always stressed, and always have the ISR turned on.
The ISR in cancer cells triggers the production of a protein called Activating Transcription Factor 4, or ATF4, which in turn triggers the action of many genes that help cancer cells survive, the study authors say. The new work shows that ATF4 also instructs the cell to release LCN2 to protect the tumor from the immune system.
“Stressed cancer cells have learned to call for help through LCN2, which shields them from the immune system,” said co-corresponding study author Thales Papagiannakopoulos, PhD, associate professor in the Department of Pathology at the NYU Grossman School of Medicine.
The research team found that LCN2 passes on the ATF4 message to switch macrophages, a type of immune cell abundant in tumors, into an “immunosuppressive” mode, which keeps cancer-killing T cells from entering the tumor.
Whereas ATF4 operates inside cancer cells, LCN2 is released outside where it can be more easily targeted by drugs, the researchers said. Therefore, they designed an antibody therapy, a lab-made version of an immune protein, to bind and block LCN2, which kept it from manipulating macrophages, letting the sidelined T cells back into tumors.
Unmasking Tumors
When the researchers team engineered mice to both develop cancer, and to lack LCN2, tumor growth slowed. That this effect happened only in mice with healthy immune systems suggested that an important role for LCN2 is to block the immune attack on tumors.
Next, the team examined tumor samples from more than 100 lung cancer patients and 30 pancreatic cancer patients. High LCN2 levels were linked to a median survival of 52 months, compared to 79 months for patients with low levels.
When treated with an antibody that blocked LCN2, tumors in mice became flooded with T cells and shrank. Combining the LCN2 antibody with an existing immunotherapy drug worked even better, extending survival in mice with aggressive lung cancer.
Story Continues
“Our results provide a clear rationale for developing therapies that target LCN2 in lung cancer patients,” said co-corresponding study author Shohei Koide, PhD, professor in the Department of Biochemistry and Molecular Pharmacology at NYU Grossman School of Medicine, and director of Cancer Biologics at Perlmutter Cancer Center. “We also want to explore whether this mechanism is active in other cancer types that resist immunotherapy.”
Along with Papagiannakopoulos and Koide, Jozef Bossowski and Ray Pillai were first authors in the Department of Pathology at NYU Langone. Also authors were in Pathology were Mari Nakamura, Ali Rashidfarrokhi, Yuan Hao, Katherine Wu, Cristina Hajdu, Sahith Rajalingam, Sarah LeBoeuf, Hortense Le , Hao Wang, Andre Moreira, Aristotelis Tsirigos, Kwok-Kin Wong, and Sergei Koralov. Authors in the Perlmutter Cancer Center were John Kilian, Takamitsu Hattori, Eliezra Glasser, and Akiko Koide.
Also authors were Angela Wong Lau, Ruxuan Li, and Ioannis Zervantonakis in the Department of Bioengineering at the University of Pittsburgh; Lidong Wang and Diane Simeone at Moores Cancer Center at the University of California, San Diego; Seungeun Lee, Jin Woo Oh, and Chan-Young Ock at Lunit Inc., Seoul, Korea; Cheolyong Joe, Hyemin Kim, and Se-Hoon Lee in the Department of Medicine in the Samsung Department of Medicine at Sungkyunkwan University School of Medicine, Seoul, Korea; Francisco Sánchez-Rivera at Department of Biology at Massachusetts Institute of Technology, and Mario Pende at Université Paris Cité, CNRS, Inserm, Institut Necker Enfants Malades (INEM) in Paris.
The study was funded by National Institutes of Health grants R37CA222504, R01CA227649, R01CA283049, R01CA262562, R01CA297605, CA271245, P50CA225450, U54CA2630001, T32EB034216, and P30CA016087. The work was also supported by American Cancer Society Research Scholar Grant RSG-17-200-01–TBE, National Science Foundation CAREER grant 2337385, the Sale Johnson Philanthropic Fund, LEO Foundation, and an ARC Fondation Postdoctorat 2 retour de l’étranger 2024 scholarship.
Dr. Papagiannakopoulos received funding from Pfizer Medical Education Group, Dracen Pharmaceuticals, Kymera Therapeutics, Bristol Myers Squibb, and Agios Pharmaceutical (not related to the submitted work). Dr. Shohei Koide is a co-founder, receives consulting fees, and holds equity in Aethon Therapeutics; is a co-founder and holds equity in Revalia Bio; and has received research funding or consulting fees from Aethon Therapeutics, Argenx BVBA, Black Diamond Therapeutics, Puretech Health, and Eisai (all outside of the current work). Papagiannakopoulos, Koide, Bossowski, and Kilian are listed as inventors on a patent related to the current study. These relationships are being managed in keeping with the policies of NYU Langone Health.
About NYU Langone Health
NYU Langone Health is a fully integrated health system that consistently achieves the best patient outcomes through a rigorous focus on quality that has resulted in some of the lowest mortality rates in the nation. Vizient Inc. has ranked NYU Langone No. 1 out of 118 comprehensive academic medical centers across the nation for four years in a row, and U.S. News & World Report recently ranked four of its clinical specialties No. 1 in the nation. NYU Langone offers a comprehensive range of medical services with one high standard of care across seven inpatient locations, its Perlmutter Cancer Center, and more than 320 outpatient locations in the New York area and Florida. The system also includes two tuition-free medical schools, in Manhattan and on Long Island, and a vast research enterprise.
Media Contact:
Gregory Williams
212-404-3500
Gregory.Williams@nyulangone.org
Cision
View original content to download multimedia:https://www.prnewswire.com/news-releases/cancer-stress-protein-helps-tumors-hide-from-immunity-302687987.html