If this is the case, why haven’t providers recommended that everybody take a titer test in the last few decades?
Because even if the antibody immunity that a vaccine offers starts to wane, that doesn’t actually mean you have no protection from measles, stressed Karan.
This is because a person’s immune system “is more than just antibodies,” he said. “You also have T cells, other components of your immune system, that are there to fight off the virus.”
So even if a titer test shows negative antibodies for measles, “It could actually still be that you’re protected through other mechanisms of your immune system, like your cellular memory.”
However, now that measles is circulating once again in the U.S., waning immunity unfortunately presents an issue. And increased measles circulation also poses a particular infection risk to immunocompromised people, those who don’t know their MMR status and babies who haven’t been able to get their two shots yet, stressed Karan.
Does my risk of waning immunity increase with age?
Yes, Karan said — an older person has a higher chance of lower titers, compared to someone whose MMR vaccine was more recent. While the length of time since you got your shots can play a factor, your immune system can also potentially weaken over time, Karan said.
An additional risk factor for older people is their birth year. Given how prevalent measles was in the U.S. before widespread vaccination, people born before 1957 aren’t routinely offered the MMR vaccine because they’re presumed to already have immunity from measles from a previous infection. The flipside of this: someone who’s 69 or older might not have actually had measles back then, so they’re lacking both infection-based immunity and the vaccine itself.
Also, people born between 1957 and 1969 may not have received two full MMR doses and should talk to their health care provider about possibly getting another vaccination.
If my blood test shows my measles immunity has waned, what then?
The most likely outcome of a titer test that shows low immunity to measles is that your provider will recommend you get another dose of the MMR vaccine.
Getting another dose of the MMR vaccine is safe even if you do have remaining immunity. “There is no harm in getting another dose of MMR vaccine if you may already be immune to measles (or mumps or rubella),” according to the CDC.
What’s more, “some providers may just give you another dose without doing the [titer] test,” Karan said.
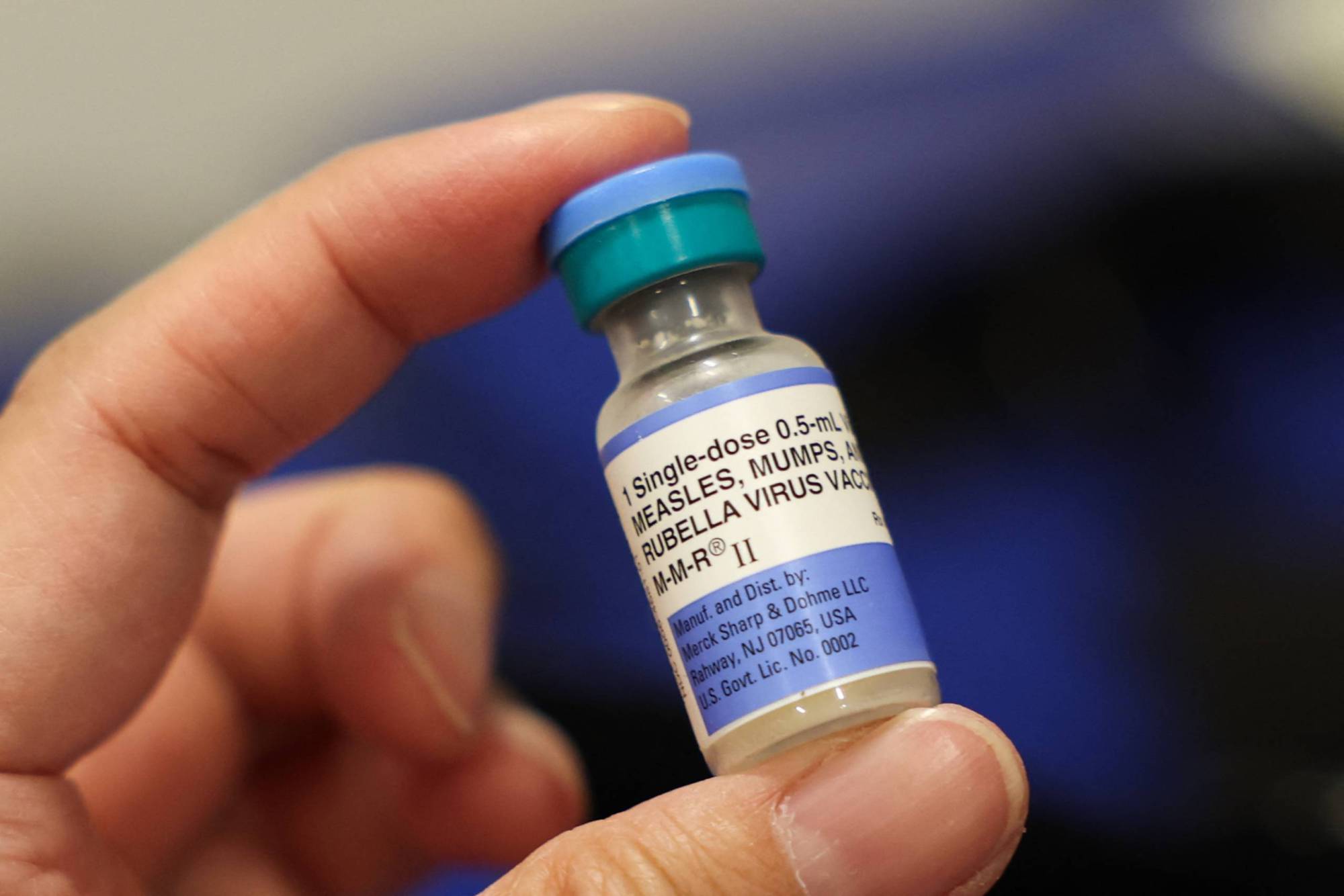 A vial of the Measles, Mumps, and Rubella (MMR) vaccination for children is displayed during an immunization event at the L.A. Care and Blue Shield of California Promise Health Plan Community Resource Center in the Panorama City neighborhood of Los Angeles, California, on Oct. 24, 2025. (Patrick T. Fallon/AFP Photo by PATRICK T. FALLON/AFP via Getty Images)
A vial of the Measles, Mumps, and Rubella (MMR) vaccination for children is displayed during an immunization event at the L.A. Care and Blue Shield of California Promise Health Plan Community Resource Center in the Panorama City neighborhood of Los Angeles, California, on Oct. 24, 2025. (Patrick T. Fallon/AFP Photo by PATRICK T. FALLON/AFP via Getty Images)
Karan noted that the titer test isn’t the only way to measure immunity, but it’s unlikely that a provider would suggest you undergo another test after getting your titers checked — and would most likely just recommend an additional MMR dose.
“Most people are not going to be able to order tests that are going to look at other kinds of immune response to measles besides just this antibody test,” he said. “So what they’ll do is they’ll just give you a dose of the vaccine. There’s no health risks.”
One situation in which a provider might not recommend an extra MMR dose: “If you’re immunocompromised to a significant degree, this might be something to discuss with your provider,” Karan said.
“There are scenarios when you don’t give people a live virus vaccine,” he said. “So that’s going to be an individual decision — and this is why the conversation has to be had with your provider before you go and do it.”
Does insurance cover a titer test?
As with all things related to health insurance in the United States, there’s no clear answer to this question.
One thing’s for sure: It’ll help if your provider can show the test is medically necessary.
While it would depend on your individual insurance, “I think the case could be made that if somebody was in a high measles area — an area that has a measles outbreak, for instance — typical public health guidance is that if you’re in an outbreak zone, either you just get another dose of MMR or you get tested,” Karan said.
Among the groups Karan said are frequently offered titer tests by providers: health care workers who’ll be treating measles patients, older and immunocompromised people and those who will be traveling to areas with measles outbreaks. “So in that sense, I would suspect that you can make the argument … that if it wasn’t covered, that it should be,” he said.
If in doubt, check with your insurer before getting the test to make sure it’ll be covered — to avoid getting stung with an unexpected bill.
Isn’t the MMR vaccine supposed to prevent measles infections altogether?
Six years of living with COVID-19 have taught us that being vaccinated against a virus doesn’t necessarily mean you won’t get infected with that virus. The COVID-19 vaccine, for example, does somewhat reduce your chances of being infected, but it also means you’re much less likely to get severely ill if you do get infected.
However, the measles vaccine is incredibly effective at protecting against infections, the CDC said, and two doses of measles vaccine are “about 97% effective” at preventing measles if you’re exposed. (One dose is “about 93% effective.”)
 According to the Centers for Disease Control and Prevention, the measles vaccine is highly effective — two doses are about 97% effective at preventing measles after exposure, while one dose is about 93% effective. (Kevin C. Cox/Getty Images)
According to the Centers for Disease Control and Prevention, the measles vaccine is highly effective — two doses are about 97% effective at preventing measles after exposure, while one dose is about 93% effective. (Kevin C. Cox/Getty Images)
These percentages mean that “about three out of 100” people vaccinated against measles will still get measles after exposure, according to the CDC. Karan noted that health officials are already seeing this in the South Carolina outbreak: “It’s a minority, but there are still a double-digit number of cases that were fully vaccinated.”
The CDC said that experts “aren’t sure why” breakthrough cases happen, but they suspect this could be due to the responsiveness of an individual’s immune system to the vaccine. It’s also possible that these vaccinated people are getting “a much higher dose of virus when they were exposed,” Karan said.
So what happens when a vaccinated person gets measles?
Regardless of why it happens, there’s at least some good news about these rare cases: “Fully vaccinated people who get measles seem more likely to have a milder illness,” the CDC said — and fully vaccinated people “seem also less likely to spread the disease to other people.”
In practice, this means that if you were vaccinated and were infected with measles, theoretically, “you would either not show symptoms at all, or you may have very mild symptoms,” Karan said.
“You would not expect someone to have a full-blown measles infection the way someone that’s not vaccinated — or who doesn’t have — immunity would have.”
All this is making me paranoid about if I even got my MMR shots. How can I check?
There’s no national organization that maintains Americans’ vaccination records. Ways that the CDC suggests to track down your own records include:
Ask your parents or caregivers for records of your childhood immunizations (or look in saved documents from your childhood, like baby books).
Consult a state immunization registry like the California Department of Public Health’s Digital Vaccine Record portal.
Ask your doctor or public health clinic, but remember that these records may only be stored for a limited time.
The CDC has a guide to tracking down your vaccination records.







