Cui, A. et al. Global and regional prevalence of vitamin D deficiency in population-based studies from 2000 to 2022: A pooled analysis of 7.9 million participants. Front. Nutr. 10, (2023).
Jiang, Z. et al. High prevalence of vitamin D deficiency in asia: A systematic review and meta-analysis. Crit Rev. Food Sci. Nutr. 63, 3602–3611 (2023).
Palacios, C. & Gonzalez, L. Is vitamin D deficiency a major global public health problem? J. Steroid Biochem. Mol. Biol. 144, 138–145 (2014).
Harju, T., Gray, B., Mavroedi, A., Farooq, A. & Reilly, J. J. Prevalence and novel risk factors for vitamin D insufficiency in elite athletes: systematic review and meta-analysis. Eur. J. Nutr. 61, 3857–3871 (2022).
Meshkin, A. et al. The global prevalence of vitamin D deficiency in the elderly: A Meta-analysis. Indian J. Orthop. 58, 223–230 (2024).
Glerup, H. et al. Hypovitaminosis D myopathy without biochemical signs of osteomalacic bone involvement. Calcif Tissue Int. 66, 419–424 (2000).
Cielen, N. et al. Vitamin D deficiency impairs skeletal muscle function in a smoking mouse model. J. Endocrinol. 229, 97–108 (2016).
Dzik, K. P. & Kaczor, J. J. Mechanisms of vitamin D on skeletal muscle function: oxidative stress, energy metabolism and anabolic state. Eur. J. Appl. Physiol. 119, 825–839 (2019).
Domingues-Faria, C. et al. Vitamin D deficiency down-regulates Notch pathway contributing to skeletal muscle atrophy in old Wistar rats. Nutr. Metab. (Lond). 11, 47 (2014).
Mizuno, T. et al. Influence of vitamin D on sarcopenia pathophysiology: A longitudinal study in humans and basic research in knockout mice. J. Cachexia Sarcopenia Muscle. 13, 2961–2973 (2022).
Yoo, J. I. et al. Comparative analysis of the association between various serum vitamin D biomarkers and sarcopenia. J. Clin. Lab. Anal. 35, e23946 (2021).
Rebolledo, B. J. et al. The association of vitamin D status in lower extremity muscle strains and core muscle injuries at the National football league combine. Arthroscopy 34, 1280–1285 (2018).
Laumonier, T. & Menetrey, J. Muscle injuries and strategies for improving their repair. J. Exp. Orthop. 3, 15 (2016).
Stauber, W. T. Factors involved in strain-induced injury in skeletal muscles and outcomes of prolonged exposures. J. Electromyogr. Kinesiol. 14, 61–70 (2004).
Kim, J. & Lee, J. Role of transforming growth factor-β in muscle damage and regeneration: focused on eccentric muscle contraction. J. Exerc. Rehabil. 13, 621–626 (2017).
Mendias, C. L. et al. Transforming growth factor-beta induces skeletal muscle atrophy and fibrosis through the induction of atrogin-1 and scleraxis. Muscle Nerve. 45, 55–59 (2012).
Li, Y. et al. Transforming growth factor-β1 induces the differentiation of myogenic cells into fibrotic cells in injured skeletal muscle: a key event in muscle fibrogenesis. Am. J. Pathol. 164, 1007–1019 (2004).
Guo, E. et al. Calcitriol ameliorates the progression of hepatic fibrosis through autophagy-related gene 16-like 1-mediated autophagy. Am. J. Med. Sci. 367, 382–396 (2024).
Potter, J. J., Liu, X., Koteish, A. & Mezey, E. 1,25-dihydroxyvitamin D3 and its nuclear receptor repress human α1(I) collagen expression and type I collagen formation. Liver Int. 33, 677–686 (2013).
Li, Y., Spataro, B. C., Yang, J., Dai, C. & Liu, Y. 1,25-dihydroxyvitamin D3 inhibits renal interstitial myofibroblast activation by inducing hepatocyte growth factor expression. Kidney Int. 68, 1500–1510 (2005).
Srikuea, R. & Hirunsai, M. TGF-β1 stimulation and VDR-dependent activation modulate calcitriol action on skeletal muscle fibroblasts and Smad signalling-associated fibrogenesis. Sci. Rep. 13, 13811 (2023).
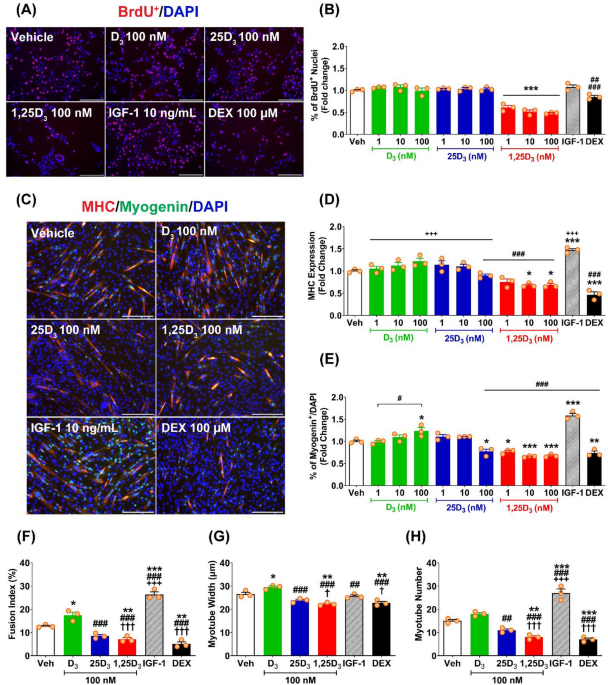
Srikuea, R., Zhang, X., Park-Sarge, O. K. & Esser, K. A. VDR and CYP27B1 are expressed in C2C12 cells and regenerating skeletal muscle: potential role in suppression of myoblast proliferation. Am. J. Physiol. Cell. Physiol. 303, C396–405 (2012).
Girgis, C. M., Clifton-Bligh, R. J., Mokbel, N., Cheng, K. & Gunton, J. E. Vitamin D signaling regulates proliferation, differentiation, and myotube size in C2C12 skeletal muscle cells. Endocrinology 155, 347–357 (2014).
Camperi, A. et al. Vitamin D and VDR in cancer cachexia and muscle regeneration. Oncotarget 8, 21778–21793 (2017).
Hirunsai, M. & Srikuea, R. Differential effects of cholecalciferol and calcitriol on muscle proteolysis and oxidative stress in angiotensin II-induced C2C12 myotube atrophy. Physiol. Rep. 12, e16011 (2024).
Teixeira, M. A. et al. Cholecalciferol (vitamin D3) has a direct protective activity against Interleukin 6-induced atrophy in C2C12 myotubes. Aging (Albany NY). 13, 4895–4910 (2021).
Sustova, H. et al. Opposing effects of 25-hydroxy- and 1α,25-dihydroxy-vitamin D3 on pro-cachectic cytokine-and cancer conditioned medium-induced atrophy in C2C12 myotubes. Acta Physiol. 226, e13269 (2019).
Olsson, K. et al. Evidence for vitamin D receptor expression and direct effects of 1α,25(OH)2D3 in human skeletal muscle precursor cells. Endocrinology 157, 98–111 (2016).
Srikuea, R. & Hirunsai, M. Effects of intramuscular administration of 1α,25(OH)2D3 during skeletal muscle regeneration on regenerative capacity, muscular fibrosis, and angiogenesis. J. Appl. Physiol. 120, 1381–1393 (2016).
Norman, A. W. From vitamin D to hormone D: fundamentals of the vitamin D endocrine system essential for good health. Am. J. Clin. Nutr. 88, 491S–499S (2008).
Srikuea, R., Hirunsai, M. & Charoenphandhu, N. Regulation of vitamin D system in skeletal muscle and resident myogenic stem cell during development, maturation, and ageing. Sci. Rep. 10, 8239 (2020).
Bass, J. J. et al. The mechanisms of skeletal muscle atrophy in response to transient knockdown of the vitamin D receptor in vivo. J. Physiol. 599, 963–979 (2021).
Tanaka, M., Kishimoto, K. N., Okuno, H., Saito, H. & Itoi, E. Vitamin D receptor gene silencing effects on differentiation of myogenic cell lines. Muscle Nerve 49, 700–708 (2014).
Das, A., Gopinath, S. D. & Arimbasseri, G. A. Systemic ablation of vitamin D receptor leads to skeletal muscle glycogen storage disorder in mice. J. Cachexia Sarcopenia Muscle. 13, 467–480 (2022).
Bass, J. J. et al. Overexpression of the vitamin D receptor (VDR) induces skeletal muscle hypertrophy. Mol. Metab. 42, 101059 (2020).
Serrano, A. L. & Muñoz-Cánoves, P. Regulation and dysregulation of fibrosis in skeletal muscle. Exp. Cell. Res. 316, 3050–3058 (2010).
Cencetti, F., Bernacchioni, C., Nincheri, P., Donati, C. & Bruni, P. Transforming growth factor-β1 induces transdifferentiation of myoblasts into myofibroblasts via up-regulation of sphingosine kinase-1/S1P3 axis. Mol. Biol. Cell. 21, 1111–1124 (2010).
Ono, Y., Sensui, H., Okutsu, S. & Nagatomi, R. Notch2 negatively regulates myofibroblastic differentiation of myoblasts. J. Cell. Physiol. 210, 358–369 (2007).
Narola, J., Pandey, S. N., Glick, A. & Chen, Y. W. Conditional expression of TGF-β1 in skeletal muscles causes endomysial fibrosis and myofibers atrophy. PLoS One 8, e79356 (2013).
Bernasconi, P. et al. Expression of transforming growth factor- β1 in dystrophic patient muscles correlates with fibrosis. Pathogenetic role of a fibrogenic cytokine. J. Clin. Invest. 96, 1137–1144 (1995).
Shi, A., Hillege, M. M. G., Wüst, R. C. I., Wu, G. & Jaspers, R. T. Synergistic short-term and long-term effects of TGF-β1 and 3 on collagen production in differentiating myoblasts. Biochem. Biophys. Res. Commun. 547, 176–182 (2021).
Bedalov, A. et al. 1,25-Dihydroxyvitamin D3 inhibition of col1a1 promoter expression in calvariae from neonatal transgenic mice. Biochim. Biophys. Acta. 1398, 285–293 (1998).
Pavlin, D. et al. Analysis of regulatory regions in the COL1A1 gene responsible for 1,25-dihydroxyvitamin D3-mediated transcriptional repression in osteoblastic cells. J. Cell. Biochem. 56, 490–501 (1994).
Slominski, A. T. et al. In vivo evidence for a novel pathway of vitamin D3 metabolism initiated by P450scc and modified by CYP27B1. FASEB J. 26, 3901–3915 (2012).
Janjetovic, Z. et al. Antifibrogenic activities of CYP11A1-derived vitamin D3-hydroxyderivatives are dependent on RORγ. Endocrinology 162, 1–14 (2021).
Chadwick, J. A. et al. Myeloid cells are capable of synthesizing aldosterone to exacerbate damage in muscular dystrophy. Hum. Mol. Genet. 25, 5167–5177 (2016).
Hirose, T., Smith, R. J. & Jetten, A. M. ROR-γ: the third member of ROR/RZR orphan receptor subfamily that is highly expressed in skeletal muscle. Biochem. Biophys. Res. Commun. 205, 1976–1983 (1994).
Fujiki, J., Maeda, N., Yamaguchi, K., Ohtsuki, Y. & Iwano, H. DNA methylation of Ad4BP/SF-1 suppresses Cyp11a1 and StAR transcripts in C2C12 myoblasts. Mol. Cell. Endocrinol. 593, 112336 (2024).
Yang, L. et al. 1,25(OH)2D3/VDR attenuates high glucose–induced epithelial –mesenchymal transition in human peritoneal mesothelial cells via the TGFβ/Smad3 pathway. Mol. Med. Rep. 15, 2273–2279 (2017).
Khalil, H. et al. Fibroblast-specific TGF-β-Smad2/3 signaling underlies cardiac fibrosis. J. Clin. Invest. 127, 3770–3783 (2017).
Wang, W., Koka, V. & Lan, H. Y. Transforming growth factor-β and Smad signalling in kidney diseases. Nephrology 10, 48–56 (2005).
Hanafusa, H. et al. Involvement of the p38 mitogen-activated protein kinase pathway in transforming growth factor-β-induced gene expression. J. Biol. Chem. 274, 27161–27167 (1999).
Rodrı́guez-Barbero, A. et al. Transforming growth factor-β1 induces collagen synthesis and accumulation via p38 mitogen-activated protein kinase (MAPK) pathway in cultured L6E9 myoblasts. FEBS Lett. 513, 282–288 (2002).
Petrocelli, J. J. et al. Skeletal muscle-specific inducible AMPKα1/α2 knockout mice develop muscle weakness, glycogen depletion, and fibrosis that persists during disuse atrophy. Am. J. Physiol. Endocrinol. Metab. 326, E50–E60 (2024).
Liu, X. et al. AMP-activated protein kinase Inhibition in fibro-adipogenic progenitors impairs muscle regeneration and increases fibrosis. J. Cachexia Sarcopenia Muscle. 14, 479–492 (2023).
Melouane, A., Yoshioka, M., Kanzaki, M. & St-Amand, J. Sparc, an EPS-induced gene, modulates the extracellular matrix and mitochondrial function via ILK/AMPK pathways in C2C12 cells. Life Sci. 229, 277–287 (2019).
Massagué, J., Cheifetz, S., Endo, T. & Nadal-Ginard, B. Type β transforming growth factor is an inhibitor of myogenic differentiation. Proc. Natl. Acad. Sci. USA 83, 8206–8210 (1986).
Abrigo, J., Rivera, J. C., Simon, F., Cabrera, D. & Cabello-Verrugio, C. Transforming growth factor type beta (TGF-β) requires reactive oxygen species to induce skeletal muscle atrophy. Cell. Signal. 28, 366–376 (2016).
Williamson, D. L., Butler, D. C. & Alway, S. E. AMPK inhibits myoblast differentiation through a PGC-1α-dependent mechanism. Am. J. Physiol. Endocrinol. Metab. 297, E304–E314 (2009).
Egawa, T. et al. AICAR-induced activation of AMPK negatively regulates myotube hypertrophy through the HSP72-mediated pathway in C2C12 skeletal muscle cells. Am. J. Physiol. Endocrinol. Metab. 306, E344–E354 (2014).
Tong, J. F., Yan, X., Zhu, M. J. & Du, M. AMP-activated protein kinase enhances the expression of muscle-specific ubiquitin ligases despite its activation of IGF-1/Akt signaling in C2C12 myotubes. J. Cell. Biochem. 108, 458–468 (2009).
Nakashima, K. & Yakabe, Y. AMPK activation stimulates myofibrillar protein degradation and expression of atrophy-related ubiquitin ligases by increasing FOXO transcription factors in C2C12 myotubes. Biosci. Biotechnol. Biochem. 71, 1650–1656 (2007).
Sanchez, A. M. et al. AMPK promotes skeletal muscle autophagy through activation of forkhead FoxO3a and interaction with Ulk1. J. Cell. Biochem. 113, 695–710 (2012).
Bolster, D. R., Crozier, S. J., Kimball, S. R. & Jefferson, L. S. AMP-activated protein kinase suppresses protein synthesis in rat skeletal muscle through down-regulated mammalian target of Rapamycin (mTOR) signaling. J. Biol. Chem. 277, 23977–23980 (2002).
Bang, W. S. et al. Relationships between vitamin D and paraspinal muscle: human data and experimental rat model analysis. Spine J. 18, 1053–1061 (2018).
Yu, M. et al. Vitamin D receptor inhibits EMT via regulation of the epithelial mitochondrial function in intestinal fibrosis. J. Biol. Chem. 296, 100531 (2021).
Ge, Y. et al. Deficiency of vitamin D receptor in keratinocytes augments dermal fibrosis and inflammation in a mouse model of HOCl-induced scleroderma. Biochem. Biophys. Res. Commun. 591, 1–6 (2022).
Ding, N. et al. A vitamin D receptor/SMAD genomic circuit gates hepatic fibrotic response. Cell 153, 601–613 (2013).
Goh, K. Y. et al. Mitoquinone ameliorates pressure overload-induced cardiac fibrosis and left ventricular dysfunction in mice. Redox Biol. 21, 101100 (2019).
Dai, D. F. et al. Mitochondrial oxidative stress mediates angiotensin II–induced cardiac hypertrophy and Gαq overexpression–induced heart failure. Circ. Res. 108, 837–846 (2011).
Song, M. et al. Augmenter of liver regeneration (ALR) gene therapy attenuates CCl4-induced liver injury and fibrosis in rats. Biochem. Biophys. Res. Commun. 415, 152–156 (2011).
Rehman, H. et al. The mitochondria-targeted antioxidant MitoQ attenuates liver fibrosis in mice. Int. J. Physiol. Pathophysiol Pharmacol. 8, 14–27 (2016).
Jain, M. et al. Mitochondrial reactive oxygen species regulate transforming growth factor-β signaling. J. Biol. Chem. 288, 770–777 (2013).
Huang, L. S. et al. Lysocardiolipin acyltransferase regulates TGF-β mediated lung fibroblast differentiation. Free Radic. Biol. Med. 112, 162–173 (2017).
Rangarajan, S. et al. Metformin reverses established lung fibrosis in a bleomycin model. Nat. Med. 24, 1121–1127 (2018).
Liao, X. et al. Fluorofenidone inhibits UUO/IRI-induced renal fibrosis by reducing mitochondrial damage. Oxid. Med. Cell. Longev. 2453617 (2022).
Yang, E. M. et al. Stanniocalcin–1 suppresses TGF–β–induced mitochondrial dysfunction and cellular fibrosis in human renal proximal tubular cells. Int. J. Mol. Med. 50, 107 (2022).
Casalena, G., Daehn, I. & Bottinger, E. Transforming growth factor-β, bioenergetics, and mitochondria in renal disease. Semin Nephrol. 32, 295–303 (2012).
Srikuea, R., Esser, K. A. & Pholpramool, C. Leukaemia inhibitory factor is expressed in rat gastrocnemius muscle after contusion and increases proliferation of rat L6 myoblasts via c-Myc signalling. Clin. Exp. Pharmacol. Physiol. 38, 501–509 (2011).
Goodman, C. A. et al. Novel insights into the regulation of skeletal muscle protein synthesis as revealed by a new nonradioactive in vivo technique. FASEB J. 25, 1028–1039 (2011).
Ge, S. X., Jung, D. & Yao, R. ShinyGO: A graphical gene-set enrichment tool for animals and plants. Bioinformatics 36, 2628–2629 (2020).