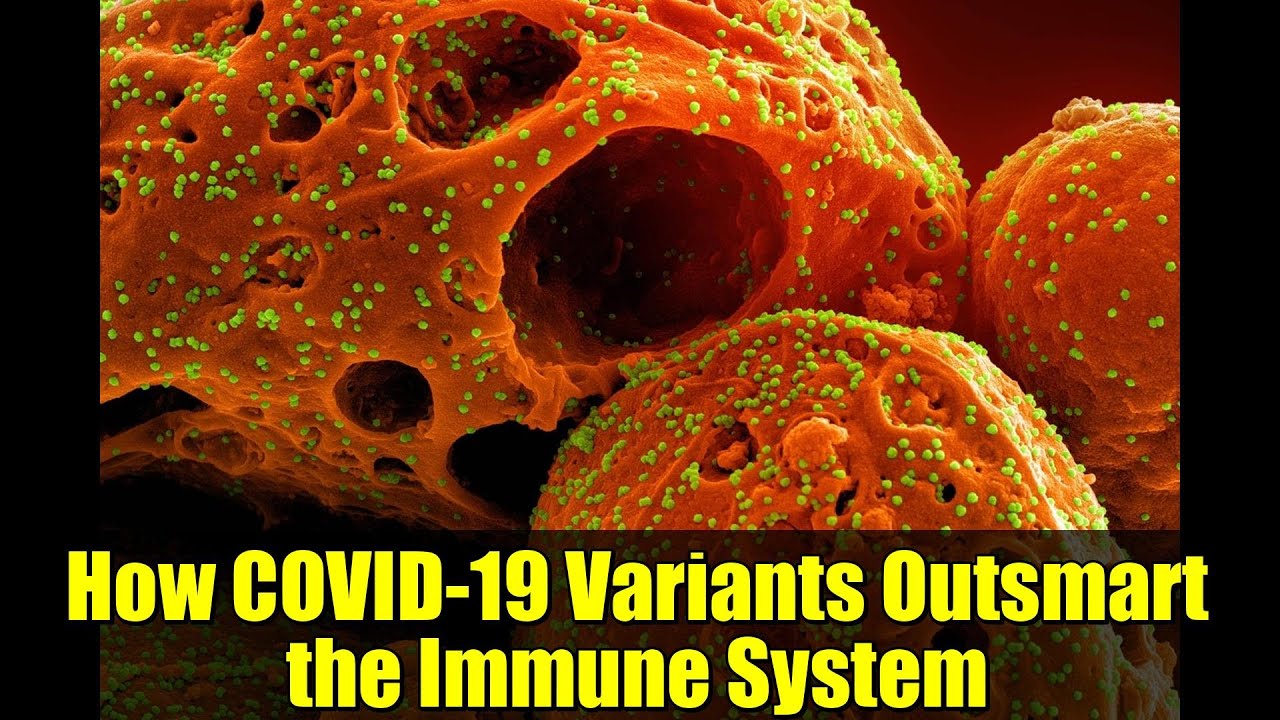
Why are COVID-19 variants like Omicron able to evade immunity? Scientists from the Icahn School of Medicine at Mount Sinai have built the most comprehensive antibody map of SARS-CoV-2 ever created. This breakthrough reveals how antibodies attach to the virus, how mutations weaken them, and what this means for the next generation of therapies and vaccines.
In this video, explore:
– How researchers mapped over 1,000 antibody–spike protein structures.
– Why most antibodies bind the virus in similar ways—and what makes that a weakness.
– How Omicron and other variants exploit these patterns to escape immune defense.
– The promising future of nanobody-based treatments that could resist viral evolution.
Keywords: COVID-19 variants, Omicron immune escape, SARS-CoV-2 antibody mapping, next-generation vaccines, nanobodies, Mount Sinai research, antiviral therapy, coronavirus evolution, immune system response, COVID-19 science insights.
Stay tuned for the latest discoveries shaping the fight against COVID-19 and future pandemics.
The CO 19 variants are smarter than we thought. They’ve learned how to slip past our immune defenses, leaving scientists racing to understand their next move. But here’s where it gets fascinating and a bit unsettling. New research from the Icon School of Medicine at Mount Si offers the most detailed explanation yet of how these viral shape shifters like Omicron managed to outweed our antibodies and what future vaccines might need to do to catch up. RT’s three big insights. The ultimate antibbody map. Mount Sinai researchers have assembled the most comprehensive structural atlas to date of SARS COV2 antibodies. This intricate map shows in fine detail how antibodies latch onto the virus’s spike protein, the key that unlocks our cells, and how even tiny viral mutations can loosen or break that grip. Shared weak points and immune evasion. After analyzing more than 1,000 antibbody spike protein structures, scientists found that most antibodies attack the virus in only a few similar structural ways. This overlap may explain why new variants such as Omicron can dodge nearly all existing antibodies so efficiently toward new kinds of therapies. The study points to multi-targeting antibodies and nanobodies, tiny powerful antibbody fragments as the next frontier in antiviral design. These could form the basis of treatments and vaccines that last longer and resist the virus’s relentless evolution. The study recently featured in cell systems involved an ambitious global effort to combine structural data from over a thousand antibbody virus interactions. For years, scientists had studied these antibbody structures individually. But until now, no one had stitched them together into a unified model. As Dr. Esher, senior author and director of the center for protein engineering and therapeutics at Mount Sinai explains, “By merging all this data, we can finally see the immune systems full landscape where it defends well and where the virus slips through. What the team saw was eyeopening. Antibodies, including many used in medical treatments, recognize nearly every visible surface on the virus’s receptor binding domain, the critical region that attaches to human cells. Yet, even with this wide coverage, the virus’s evolution is like a chess game where every move shifts the board. Small mutations now found in newer variants can weaken the effectiveness of nearly all known antibodies. Strikingly, many antibodies that differ genetically still lock onto the virus in nearly the same way. That structural similarity means the virus only needs to mutate in a few critical places to escape a wide range of immune attacks. This convergence may be one of the cleverest survival tricks nature has ever played. The researchers also highlighted the promise of nanobodies, tiny robust antibbody pieces derived from animals like llamas and camels. Unlike standard antibodies, nanobodies can reach deep into hidden pockets of the spike protein that rarely mutate. This makes them promising candidates for next generation COVID 19 treatments designed to endure as the virus continues to evolve. Dr. Sher emphasized that current antibbody therapies, while life-saving, are not the endgame. These antibodies have done wonders, but the virus learns fast. To stay ahead, our treatments must become multi-sight and multi-layered, hitting the virus in several places at once, so it has nowhere to hide. led researcher Frank Zerwe Fun added that identifying overlapping antibbody targets could allow future drugs to attack both current and yet to emerge variants in one strike. Another key takeaway is that this research doesn’t mean vaccines or natural immunity have failed. They still protect against severe disease. The body’s defense system is complex and multi-armed. Antibodies are only one part of that arsenal. Still, the study serves as a wake-up call. As the virus keeps evolving, our long-term defense will depend on how well we adapt our tools to meet its growing sophistication. The Mount Si team plans to extend this massive structural analysis to other viruses, hoping to uncover universal principles of immune evasion. Ultimately, their goal is to design antiviral drugs and vaccines that can endure over time. immune weapons that don’t just react to viral evolution, but anticipate it. As co-author Dr. Adalfo Garcia Austri put it, “The immune system is an incredible problem solver, but the virus is no less ingenious. Our job is to find its weak spots faster than it can find ours.” Using their open access data set and interactive web tool, scientists worldwide can now explore antibbody virus interactions in unprecedented detail. A community-driven effort to push global antiviral research forward. And this is the part most people miss. Understanding how CO 19 variants escape doesn’t signal defeat. It shows exactly where to focus the next generation of vaccines and treatments. If the virus is evolving like a master strategist, perhaps the real question is whether our science can learn to think a move ahead. So, what do you think? Should vaccine design focus more on multi-target antibodies and nanobbody- based therapies? Or do you believe current vaccine strategies are enough to stay ahead of future variants?