Veldhoen, M., Hocking, R. J., Atkins, C. J., Locksley, R. M. & Stockinger, B. TGFβ in the context of an inflammatory cytokine milieu supports de novo differentiation of IL-17-producing T cells. Immunity 24, 179–189 (2006).
Bettelli, E. et al. Reciprocal developmental pathways for the generation of pathogenic effector TH17 and regulatory T cells. Nature 441, 235–238 (2006).
Mangan, P. R. et al. Transforming growth factor-β induces development of the TH17 lineage. Nature 441, 231–234 (2006).
Ivanov, I. I. et al. The orphan nuclear receptor RORγt directs the differentiation program of proinflammatory IL-17+ T helper cells. Cell 126, 1121–1133 (2006). This work presents the initial identification of RORγt as the master regulator of the TH17 cell lineage.
Goto, Y. et al. Segmented filamentous bacteria antigens presented by intestinal dendritic cells drive mucosal TH17 cell differentiation. Immunity 40, 594–607 (2014).
Schnell, A., Littman, D. R. & Kuchroo, V. K. TH17 cell heterogeneity and its role in tissue inflammation. Nat. Immunol. 24, 19–29 (2023).
Stockinger, B. & Omenetti, S. The dichotomous nature of T helper 17 cells. Nat. Rev. Immunol. 17, 535–544 (2017).
McGeachy, M. J. et al. TGF-β and IL-6 drive the production of IL-17 and IL-10 by T cells and restrain TH-17 cell-mediated pathology. Nat. Immunol. 8, 1390–1397 (2007). This study reveals that whereas TGFβ1 plus IL-6 polarizes TH17 cells towards a regulatory, IL-10-producing phenotype, the addition of IL-23 enables their pathogenicity and capacity to drive EAE.
Brockmann, L. et al. Intestinal microbiota-specific TH17 cells possess regulatory properties and suppress effector T cells via c-MAF and IL-10. Immunity 56, 2719–2735.e7 (2023).
Ahern, P. P. et al. Interleukin-23 drives intestinal inflammation through direct activity on T cells. Immunity 33, 279–288 (2010).
Ghoreschi, K. et al. Generation of pathogenic TH17 cells in the absence of TGF-β signalling. Nature 467, 967–971 (2010).
Zielinski, C. E. et al. Pathogen-induced human TH17 cells produce IFN-γ or IL-10 and are regulated by IL-1β. Nature 484, 514–518 (2012).
Wu, B. et al. The TGF-β superfamily cytokine activin-A is induced during autoimmune neuroinflammation and drives pathogenic TH17 cell differentiation. Immunity 54, 308–323.e6 (2021).
Lee, Y. et al. Induction and molecular signature of pathogenic TH17 cells. Nat. Immunol. 13, 991–999 (2012).
Langrish, C. L. et al. IL-23 drives a pathogenic T cell population that induces autoimmune inflammation. J. Exp. Med. 201, 233–240 (2005). This study was the first to demonstrate that IL-23 drives the expansion of a pathogenic, IL-17-producing CD4+ T cell population, with a cytokine profile distinct from TH1 cells.
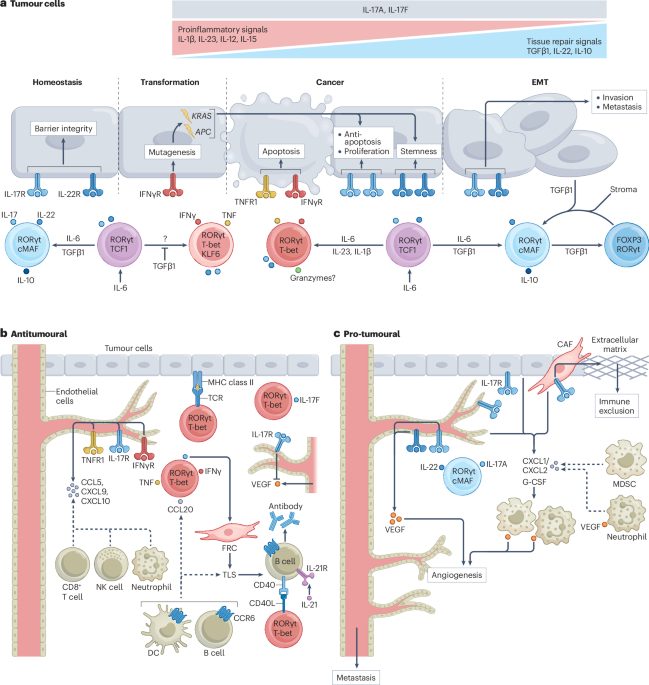
Zou, W. & Restifo, N. P. TH17 cells in tumour immunity and immunotherapy. Nat. Rev. Immunol. 10, 248–256 (2010).
Anvar, M. T. et al. TH17 cell function in cancers: immunosuppressive agents or anti-tumor allies? Cancer Cell Int. 24, 355 (2024).
Ciofani, M. et al. A validated regulatory network for TH17 cell specification. Cell 151, 289–303 (2012).
Yosef, N. et al. Dynamic regulatory network controlling TH17 cell differentiation. Nature 496, 461–468 (2013).
Gaublomme, J. T. et al. Single-cell genomics unveils critical regulators of TH17 cell pathogenicity. Cell 163, 1400–1412 (2015).
Wagner, A. et al. Metabolic modeling of single TH17 cells reveals regulators of autoimmunity. Cell 184, 4168–4185.e21 (2021).
Hu, L. et al. Proximal and distal regions of pathogenic TH17 related chromatin loci are sequentially accessible during pathogenicity of TH17. Front. Immunol. 13, 864314 (2022).
Thakore, P. I. et al. BACH2 regulates diversification of regulatory and proinflammatory chromatin states in TH17 cells. Nat. Immunol. 25, 1395–1410 (2024).
Karmaus, P. W. F. et al. Metabolic heterogeneity underlies reciprocal fates of TH17 cell stemness and plasticity. Nature 565, 101–105 (2019). This study demonstrates that mTORC1 activity in TH17 cells acts as a central switch that controls their plasticity.
Schnell, A. et al. Stem-like intestinal TH17 cells give rise to pathogenic effector T cells during autoimmunity. Cell 184, 6281–6298.e23 (2021).
Hanahan, D. Hallmarks of cancer: new dimensions. Cancer Discov. 12, 31–46 (2022).
Mills, K. H. G. IL-17 and IL-17-producing cells in protection versus pathology. Nat. Rev. Immunol. 23, 38–54 (2023).
Sun, K. et al. scRNA-seq of gastric tumor shows complex intercellular interaction with an alternative T cell exhaustion trajectory. Nat. Comm. 13, 4943 (2022).
McAllister, F. et al. Oncogenic Kras activates a hematopoietic-to-epithelial IL-17 signaling axis in preinvasive pancreatic neoplasia. Cancer Cell 25, 621–637 (2014).
Chang, S. H. et al. T helper 17 cells play a critical pathogenic role in lung cancer. Proc. Natl Acad. Sci. USA 111, 5664–5669 (2014).
Zhang, Q. et al. Interleukin-17 promotes formation and growth of prostate adenocarcinoma in mouse models. Cancer Res. 72, 2589–2599 (2012).
Chandra, V. et al. Gut epithelial Interleukin-17 receptor A signaling can modulate distant tumors growth through microbial regulation. Cancer Cell 42, 85–100.e6 (2024).
Wang, K. et al. Interleukin-17 receptor A signaling in transformed enterocytes promotes early colorectal tumorigenesis. Immunity 41, 1052–1063 (2014). This study shows that malignant transformation in epithelial cells is a prerequisite for pro-tumorigenic IL-17 signalling.
Numasaki, M. et al. Interleukin-17 promotes angiogenesis and tumor growth. Blood 101, 2620–2627 (2003).
McCuaig, S. et al. The interleukin 22 pathway interacts with mutant KRAS to promote poor prognosis in colon cancer. Clin. Cancer Res. 26, 4313–4325 (2020).
Khosravi, N. et al. IL22 promotes Kras-mutant lung cancer by induction of a protumor immune response and protection of stemness properties. Cancer Immunol. Res. 6, 788–797 (2018).
Kryczek, I. et al. IL-22+CD4+ T cells promote colorectal cancer stemness via STAT3 transcription factor activation and induction of the methyltransferase DOT1L. Immunity 40, 772–784 (2014).
Perusina Lanfranca, M. et al. Interleukin 22 signaling regulates acinar cell plasticity to promote pancreatic tumor development in mice. Gastroenterology 158, 1417–1432.e11 (2020).
Zhang, Y. et al. Immune cell production of interleukin 17 induces stem cell features of pancreatic intraepithelial neoplasia cells. Gastroenterology 155, 210–223.e3 (2018).
Salazar, Y. et al. Microenvironmental TH9 and TH17 lymphocytes induce metastatic spreading in lung cancer. J. Clin. Invest. 130, 3560–3575 (2020).
Yao, J. et al. Single-cell transcriptomic analysis in a mouse model deciphers cell transition states in the multistep development of esophageal cancer. Nat. Comm. 11, 3715 (2020).
Xing, C. et al. TH17 cells regulate chemokine expression in epithelial cells through C/EBPβ and dictate host sensitivity to colitis and cancer immunity. Sci. Adv. 11, eads3530 (2025).
Gronke, K. et al. Interleukin-22 protects intestinal stem cells against genotoxic stress. Nature 566, 249–253 (2019).
Perez, L. G. et al. TGF-β signaling in TH17 cells promotes IL-22 production and colitis-associated colon cancer. Nat. Comm. 11, 2608 (2020).
Fesneau, O. et al. An intestinal TH17 cell-derived subset can initiate cancer. Nat. Immunol. 25, 1637–1649 (2024). This work identifies a novel TH17 cell subset that arises following the loss of TGFβ1 signalling and can directly initiate intestinal tumorigenesis via IFNγ.
Wu, S. et al. A human colonic commensal promotes colon tumorigenesis via activation of T helper type 17 T cell responses. Nat. Med. 15, 1016–1022 (2009). This study was the first to reveal a causal link between the colonization of a gut pathobiont and IL-17-driven tumorigenesis, establishing the microbiota as a direct instigator of pro-tumorigenic TH17 cell activity.
Wang, L., Yi, T., Zhang, W., Pardoll, D. M. & Yu, H. IL-17 enhances tumor development in carcinogen-induced skin cancer. Cancer Res. 70, 10112–10120 (2010).
Benevides, L. et al. IL17 promotes mammary tumor progression by changing the behavior of tumor cells and eliciting tumorigenic neutrophils recruitment. Cancer Res. 75, 3788–3799 (2015).
He, D. et al. IL-17 promotes tumor development through the induction of tumor promoting microenvironments at tumor sites and myeloid-derived suppressor cells. J. Immunol. 184, 2281–2288 (2010).
Coffelt, S. B. et al. IL-17-producing γδ T cells and neutrophils conspire to promote breast cancer metastasis. Nature 522, 345–348 (2015).
Chung, A. S. et al. An interleukin-17-mediated paracrine network promotes tumor resistance to anti-angiogenic therapy. Nat. Med. 19, 1114–1123 (2013). This mechanistic study shows that TH17 cell-driven recruitment of neutrophils into the TME leads to anti-VEGF therapy resistance.
Numasaki, M. et al. IL-17 enhances the net angiogenic activity and in vivo growth of human non-small cell lung cancer in SCID mice through promoting CXCR-2-dependent angiogenesis. J. Immunol. 175, 6177–6189 (2005).
Amicarella, F. et al. Dual role of tumour-infiltrating T helper 17 cells in human colorectal cancer. Gut 66, 692–704 (2017).
Kryczek, I. et al. Phenotype, distribution, generation, and functional and clinical relevance of TH17 cells in the human tumor environments. Blood 114, 1141–1149 (2009).
Martin-Orozco, N. et al. T helper 17 cells promote cytotoxic T cell activation in tumor immunity. Immunity 31, 787–798 (2009).
Muranski, P. et al. Tumor-specific TH17-polarized cells eradicate large established melanoma. Blood 112, 362–373 (2008). This work presents the first evidence that tumour antigen-specific, TCR-engineered TH17 cells can protect against established melanoma.
Kadomoto, S., Izumi, K. & Mizokami, A. The CCL20–CCR6 axis in cancer progression. Int. J. Mol. Sci. 21, 5186 (2020).
Muranski, P. et al. TH17 cells are long lived and retain a stem cell-like molecular signature. Immunity 35, 972–985 (2011). This study demonstrates that TH17 cells, unlike TH1 cells, maintain stem-like properties that support long-term persistence within the TME and durable antitumour immunity.
Bowers, J. S. et al. TH17 cells are refractory to senescence and retain robust antitumor activity after long-term ex vivo expansion. JCI Insight 2, e90772 (2017).
Peters, A. et al. TH17 cells induce ectopic lymphoid follicles in central nervous system tissue inflammation. Immunity 35, 986–996 (2011).
Pikor, Natalia B. et al. Integration of TH17- and lymphotoxin-derived signals initiates meningeal-resident stromal cell remodeling to propagate neuroinflammation. Immunity 43, 1160–1173 (2015).
Rangel-Moreno, J. et al. The development of inducible bronchus-associated lymphoid tissue depends on IL-17. Nat. Immunol. 12, 639–646 (2011).
Eddens, T. et al. Pneumocystis -driven inducible bronchus-associated lymphoid tissue formation requires TH2 and TH17 immunity. Cell Rep. 18, 3078–3090 (2017).
Schumacher, T. N. & Thommen, D. S. Tertiary lymphoid structures in cancer. Science 375, eabf9419 (2022).
Majumder, S. et al. IL-17 metabolically reprograms activated fibroblastic reticular cells for proliferation and survival. Nat. Immunol. 20, 534–545 (2019).
Cole, A. C. et al. Adoptively transferred TH17 cells cooperate with host B cells to achieve durable tumor immunity. Cancer Cell 43, 1697–1713.e8 (2025).
Corgnac, S. et al. CD103+CD8+ TRM cells accumulate in tumors of anti-PD-1-responder lung cancer patients and are tumor-reactive lymphocytes enriched with TC17. Cell Rep. Med. 1, 100127 (2020).
Boulch, M. et al. Tumor-intrinsic sensitivity to the pro-apoptotic effects of IFN-γ is a major determinant of CD4+ CAR T-cell antitumor activity. Nat. Cancer 4, 968–983 (2023).
Braumüller, H. et al. T-helper-1-cell cytokines drive cancer into senescence. Nature 494, 361–365 (2013).
Kruse, B. et al. CD4+ T cell-induced inflammatory cell death controls immune-evasive tumours. Nature 618, 1033–1040 (2023).
Rizzo, A. et al. Smad7 induces plasticity in tumor-infiltrating TH17 cells and enables TNF-α-mediated killing of colorectal cancer cells. Carcinogenesis 35, 1536–1546 (2014).
Kebir, H. et al. Human TH17 lymphocytes promote blood-brain barrier disruption and central nervous system inflammation. Nat. Med. 13, 1173–1175 (2007).
Jamann, H. et al. Contact-dependent granzyme B-mediated cytotoxicity of TH17-polarized cells toward human oligodendrocytes. Front. Immunol. 13, 850616 (2022).
Bailey, S. R. et al. Human CD26high T cells elicit tumor immunity against multiple malignancies via enhanced migration and persistence. Nat. Comm. 8, 1961 (2017).
Chalmin, F. et al. Stat3 and Gfi-1 transcription factors control TH17 cell immunosuppressive activity via the regulation of ectonucleotidase expression. Immunity 36, 362–373 (2012).
Downs-Canner, S. et al. Suppressive IL-17A+Foxp3+ and ex-TH17 IL-17AnegFoxp3+ Treg cells are a source of tumour-associated Treg cells. Nat. Comm. 8, 14649 (2017). This fate-mapping study shows that immunosuppressive tumour niches can drive the transdifferentiation of tumour-resident TH17 cells into Treg cells.
Mucciolo, G. et al. IL17A critically shapes the transcriptional program of fibroblasts in pancreatic cancer and switches on their protumorigenic functions. Proc. Natl Acad. Sci. USA 118, e2020395118 (2021).
Chen, X. et al. IL-17–induced HIF1α drives resistance to anti–PD-L1 via fibroblast-mediated immune exclusion. J. Exp. Med. 219, e20210693 (2022).
Zhang, Y. et al. Interleukin-17–induced neutrophil extracellular traps mediate resistance to checkpoint blockade in pancreatic cancer. J. Exp. Med. 217, e20190354 (2020).
Zhou, Y. et al. Interleukin-17F suppressed colon cancer by enhancing caspase 4 mediated pyroptosis of endothelial cells. Sci. Rep. 14, 18363 (2024).
Tong, Z. et al. A protective role by interleukin-17F in colon tumorigenesis. PLoS One 7, e34959 (2012).
Picard, F. S. R. et al. IL-17A-producing CD8+ T cells promote PDAC via induction of inflammatory cancer-associated fibroblasts. Gut 72, 1510 (2023).
Neuhaus, F. et al. Reciprocal crosstalk between Th17 and mesothelial cells promotes metastasis-associated adhesion of ovarian cancer cells. Clin. Transl. Med. 14, e1604 (2024).
Kryczek, I. et al. Human TH17 cells are long-lived effector memory cells. Sci. Transl. Med. 3, 104ra100 (2011).
Buck, M. ichaelD. et al. Mitochondrial dynamics controls T cell fate through metabolic programming. Cell 166, 63–76 (2016).
Baixauli, F. et al. An LKB1–mitochondria axis controls TH17 effector function. Nature 610, 555–561 (2022).
Hong, H. S. et al. OXPHOS promotes apoptotic resistance and cellular persistence in TH17 cells in the periphery and tumor microenvironment. Sci. Immunol. 7, eabm8182 (2022).
Lin, C.-H. et al. Selective IL-27 production by intestinal regulatory T cells permits gut-specific regulation of TH17 cell immunity. Nat. Immunol. 24, 2108–2120 (2023).
Knochelmann, H. M. et al. IL6 fuels durable memory for TH17 cell–mediated responses to tumors. Cancer Res. 80, 3920–3932 (2020).
Grivennikov, S. I. et al. Adenoma-linked barrier defects and microbial products drive IL-23/IL-17-mediated tumour growth. Nature 491, 254–258 (2012). This study shows that breakdown of the intestinal epithelial barrier in early adenomas permits bacterial translocation, which drives tumour-promoting TH17 cell-mediated inflammation.
Dmitrieva-Posocco, O. et al. Cell-type-specific responses to interleukin-1 control microbial invasion and tumor-elicited inflammation in colorectal cancer. Immunity 50, 166–180.e7 (2019).
Voigt, C. et al. Cancer cells induce interleukin-22 production from memory CD4+ T cells via interleukin-1 to promote tumor growth. Proc. Natl Acad. Sci. USA 114, 12994–12999 (2017).
Laoui, D. et al. The tumour microenvironment harbours ontogenically distinct dendritic cell populations with opposing effects on tumour immunity. Nat. Comm. 7, 13720 (2016).
Mangani, D. et al. Transcription factor TCF1 binds to RORγt and orchestrates a regulatory network that determines homeostatic TH17 cell state. Immunity 57, 2565–2582.e6 (2024).
West, N. R., McCuaig, S., Franchini, F. & Powrie, F. Emerging cytokine networks in colorectal cancer. Nat. Rev. Immunol. 15, 615–629 (2015).
Chatterjee, S. et al. Reducing CD73 expression by IL1β-programmed TH17 cells improves immunotherapeutic control of tumors. Cancer Res. 74, 6048–6059 (2014).
Minns, D. et al. The neutrophil antimicrobial peptide cathelicidin promotes TH17 differentiation. Nat. Comm. 12, 1285 (2021).
Walch-Rückheim, B. et al. Stromal fibroblasts induce CCL20 through IL6/C/EBPβ to support the recruitment of TH17 cells during cervical cancer progression. Cancer Res. 75, 5248–5259 (2015).
Yu, Q., Lou, X.-M. & He, Y. Preferential recruitment of TH17 cells to cervical cancer via CCR6–CCL20 pathway. PLoS ONE 10, e0120855 (2015).
Guedan, S. et al. ICOS-based chimeric antigen receptors program bipolar TH17/TH1 cells. Blood 124, 1070–1080 (2014).
Dhodapkar, K. M. et al. Dendritic cells mediate the induction of polyfunctional human IL17-producing cells (TH17-1 cells) enriched in the bone marrow of patients with myeloma. Blood 112, 2878–2885 (2008).
Wyatt, M. M. et al. Augmenting TCR signal strength and ICOS costimulation results in metabolically fit and therapeutically potent human CAR TH17 cells. Mol. Ther. 31, 2120–2131 (2023).
Sun, J. et al. Tumor exosome promotes TH17 cell differentiation by transmitting the lncRNA CRNDE-h in colorectal cancer. Cell Death Dis. 12, 123 (2021).
Guo, D. et al. Exosomes from heat-stressed tumour cells inhibit tumour growth by converting regulatory T cells to TH17 cells via IL-6. Immunology 154, 132–143 (2018).
Liu, F., Bu, Z., Zhao, F. & Xiao, D. Increased T-helper 17 cell differentiation mediated by exosome-mediated microRNA-451 redistribution in gastric cancer infiltrated T cells. Cancer Sci. 109, 65–73 (2018).
Zhou, J. et al. Exosomes released from tumor-associated macrophages transfer miRNAs that induce a Treg/TH17 cell imbalance in epithelial ovarian cancer. Cancer Immunol. Res. 6, 1578–1592 (2018).
Huang, Y. et al. CD4+ and CD8+ T cells have opposing roles in breast cancer progression and outcome. Oncotarget 6, 17462–17478 (2015).
Blatner, N. R. et al. Expression of RORαt marks a pathogenic regulatory T cell subset in human colon cancer. Sci. Transl. Med. 4, 164ra159 (2012).
Rizzo, A. et al. Smad7 expression in T cells prevents colitis-associated cancer. Cancer Res. 71, 7423–7432 (2011).
Koncina, E. et al. IL1R1+ cancer-associated fibroblasts drive tumor development and immunosuppression in colorectal cancer. Nat. Comm. 14, 4251 (2023).
Hirota, K. et al. Fate mapping of IL-17-producing T cells in inflammatory responses. Nat. Immunol. 12, 255–263 (2011). This study presents the first use of Il17a fate-reporter mice, demonstrating plasticity within the TH17 cell compartment as IL-17+ TH17 cells act as a reservoir for IFNγ+ TH17 cells during EAE.
Wong, S. H. et al. Gavage of fecal samples from patients with colorectal cancer promotes intestinal carcinogenesis in germ-free and conventional mice. Gastroenterology 153, 1621–1633.e6 (2017).
Long, X. et al. Peptostreptococcus anaerobius promotes colorectal carcinogenesis and modulates tumour immunity. Nat. Microbiol. 4, 2319–2330 (2019).
Cao, Y. et al. Enterotoxigenic Bacteroides fragilis promotes intestinal inflammation and malignancy by inhibiting exosome-packaged miR-149-3p. Gastroenterology 161, 1552–1566.e12 (2021).
Brennan, C. A. et al. Fusobacterium nucleatum drives a pro-inflammatory intestinal microenvironment through metabolite receptor-dependent modulation of IL-17 expression. Gut Microbes 13, 1987780 (2021).
Zhao, L. et al. Parvimonas micra promotes colorectal tumorigenesis and is associated with prognosis of colorectal cancer patients. Oncogene 41, 4200–4210 (2022).
Xing, C. et al. Microbiota regulate innate immune signaling and protective immunity against cancer. Cell Host Microbe 29, 959–974.e7 (2021).
Omenetti, S. et al. The intestine harbors functionally distinct homeostatic tissue-resident and inflammatory TH17 cells. Immunity 51, 77–89.e76 (2019). This study maps the regulatory networks which control intestinal TH17 cells, revealing that functionally distinct subsets are differentially induced by commensal and pathogenic bacteria.
Chung, L. et al. Bacteroides fragilis toxin coordinates a pro-carcinogenic inflammatory cascade via targeting of colonic epithelial cells. Cell Host Microbe 23, 203–214.e5 (2018).
Dejea, C. M. et al. Patients with familial adenomatous polyposis harbor colonic biofilms containing tumorigenic bacteria. Science 359, 592–597 (2018).
Nejman, D. et al. The human tumor microbiome is composed of tumor type-specific intracellular bacteria. Science 368, 973–980 (2020).
Tanoue, T. et al. A defined commensal consortium elicits CD8 T cells and anti-cancer immunity. Nature 565, 600–605 (2019).
Viaud, S. et al. Cyclophosphamide induces differentiation of TH17 cells in cancer patients. Cancer Res. 71, 661–665 (2011).
Viaud, S. et al. The intestinal microbiota modulates the anticancer immune effects of cyclophosphamide. Science 342, 971–976 (2013).
Yang, Y. et al. Focused specificity of intestinal TH17 cells towards commensal bacterial antigens. Nature 510, 152–156 (2014).
Kalaora, S. et al. Identification of bacteria-derived HLA-bound peptides in melanoma. Nature 592, 138–143 (2021).
Naghavian, R. et al. Microbial peptides activate tumour-infiltrating lymphocytes in glioblastoma. Nature 617, 807–817 (2023).
Najar, T. A. et al. Microbiota-induced plastic T cells enhance immune control of antigen-sharing tumors. Preprint at bioRxiv https://doi.org/10.1101/2024.08.12.607605 (2024).
Kostic, A. D. et al. Fusobacterium nucleatum potentiates intestinal tumorigenesis and modulates the tumor-immune microenvironment. Cell Host Microbe 14, 207–215 (2013).
Rubinstein, M. R. et al. Fusobacterium nucleatum promotes colorectal carcinogenesis by modulating E-cadherin/β-catenin signaling via its FadA adhesin. Cell Host Microbe 14, 195–206 (2013).
Kostic, A. D. et al. Genomic analysis identifies association of Fusobacterium with colorectal carcinoma. Genome Res. 22, 292–298 (2012).
Ternes, D. et al. The gut microbial metabolite formate exacerbates colorectal cancer progression. Nat. Metab. 4, 458–475 (2022).
Han, J.-X. et al. Microbiota-derived tryptophan catabolites mediate the chemopreventive effects of statins on colorectal cancer. Nat. Microbiol. 8, 919–933 (2023).
Song, X. et al. Microbial bile acid metabolites modulate gut RORγ+ regulatory T cell homeostasis. Nature 577, 410–415 (2020).
Paik, D. et al. Human gut bacteria produce TH17-modulating bile acid metabolites. Nature 603, 907–912 (2022).
Hang, S. et al. Bile acid metabolites control TH17 and Treg cell differentiation. Nature 576, 143–148 (2019).
Wilck, N. et al. Salt-responsive gut commensal modulates TH17 axis and disease. Nature 551, 585–589 (2017).
Wu, C. et al. Induction of pathogenic TH17 cells by inducible salt-sensing kinase SGK1. Nature 496, 513–517 (2013).
Kleinewietfeld, M. et al. Sodium chloride drives autoimmune disease by the induction of pathogenic TH17 cells. Nature 496, 518–522 (2013).
Yang, W. et al. Intestinal microbiota-derived short-chain fatty acids regulation of immune cell IL-22 production and gut immunity. Nat. Comm. 11, 4457 (2020).
Chen, L. et al. Microbiota metabolite butyrate differentially regulates TH1 and TH17 cells’ differentiation and function in induction of colitis. Inflamm. Bowel Dis. 25, 1450–1461 (2019).
Luu, M. et al. The short-chain fatty acid pentanoate suppresses autoimmunity by modulating the metabolic-epigenetic crosstalk in lymphocytes. Nat. Comm. 10, 760 (2019).
Park, J. et al. Short-chain fatty acids induce both effector and regulatory T cells by suppression of histone deacetylases and regulation of the mTOR–S6K pathway. Mucosal Immunol. 8, 80–93 (2015).
Deng, Z. et al. Enterobacteria-secreted particles induce production of exosome-like S1P-containing particles by intestinal epithelium to drive TH17-mediated tumorigenesis. Nat. Comm. 6, 6956 (2015).
Briukhovetska, D. et al. Interleukins in cancer: from biology to therapy. Nat. Rev. Cancer 21, 481–499 (2021).
Xiao, S. et al. Small-molecule RORγt antagonists inhibit T helper 17 cell transcriptional network by divergent mechanisms. Immunity 40, 477–489 (2014).
Ling, L. et al. Circulating and tumor-infiltrating mucosal associated invariant T (MAIT) cells in colorectal cancer patients. Sci. Rep. 6, 20358 (2016).
Wu, L. et al. Niche-selective inhibition of pathogenic TH17 cells by targeting metabolic redundancy. Cell 182, 641–654.e20 (2020).
Chao, Y.-Y. et al. Human TH17 cells engage gasdermin E pores to release IL-1α on NLRP3 inflammasome activation. Nat. Immunol. 24, 295–308 (2023).
Park, E. et al. Integrin α3 promotes TH17 cell polarization and extravasation during autoimmune neuroinflammation. Sci. Immunol. 8, eadg7597 (2023).
Du, F. et al. Inflammatory TH17 cells express integrin αvβ3 for pathogenic function. Cell Rep. 16, 1339–1351 (2016).
Duc, D. et al. Disrupting myelin-specific TH17 cell gut homing confers protection in an adoptive transfer experimental autoimmune encephalomyelitis. Cell Rep. 29, 378–390.e4 (2019).
Feagan, B. G. et al. Vedolizumab as induction and maintenance therapy for ulcerative colitis. N. Engl. J. Med. 369, 699–710 (2013).
Van De Veerdonk, F. L. et al. The macrophage mannose receptor induces IL-17 in response to Candida albicans. Cell Host Microbe 5, 329–340 (2009).
Son, S. et al. Induction of T-helper-17-cell-mediated anti-tumour immunity by pathogen-mimicking polymer nanoparticles. Nat. Biomed. Eng. 7, 72–84 (2022).
Anker, J. F. et al. Multi-faceted immunomodulatory and tissue-tropic clinical bacterial isolate potentiates prostate cancer immunotherapy. Nat. Comm. 9, 1591 (2018).
Harbour, S. N. et al. TH17 cells require ongoing classic IL-6 receptor signaling to retain transcriptional and functional identity. Sci. Immunol. 5, eaaw2262 (2020).
Gao, Y. et al. Transcriptional profiling identifies caspase-1 as a T cell–intrinsic regulator of TH17 differentiation. J. Exp. Med. 217, e20190476 (2020).
Zhang, Y. et al. Anti-CD40-induced inflammatory E-cadherin+ dendritic cells enhance T cell responses and antitumour immunity in murine Lewis lung carcinoma. J. Exp. Clin. Cancer Res. 34, 11 (2015).
Vedunova, M. et al. DC vaccines loaded with glioma cells killed by photodynamic therapy induce TH17 anti-tumor immunity and provide a four-gene signature for glioma prognosis. Cell Death Dis. 13, 1062 (2022).
Luo, Y. et al. TH17-inducing dendritic cell vaccines stimulate effective CD4 T cell-dependent antitumor immunity in ovarian cancer that overcomes resistance to immune checkpoint blockade. J. Immunother. Cancer 11, e007661 (2023).
Block, M. S. et al. TH17-inducing autologous dendritic cell vaccination promotes antigen-specific cellular and humoral immunity in ovarian cancer patients. Nat. Comm. 11, 5173 (2020). This phase I clinical trial shows that an autologous DC vaccine can induce protective, tumour antigen-specific TH17 cell responses in ovarian cancer.
Izumi, G. et al. CD11b+ lung dendritic cells at different stages of maturation induce TH17 or TH2 differentiation. Nat. Comm. 12, 5029 (2021).
Xu, K. et al. Glycolytic ATP fuels phosphoinositide 3-kinase signaling to support effector T helper 17 cell responses. Immunity 54, 976–987.e7 (2021).
Hochrein, S. M. et al. The glucose transporter GLUT3 controls T helper 17 cell responses through glycolytic-epigenetic reprogramming. Cell Metab. 34, 516–532.e11 (2022).
Chen, C. et al. Vitamin B5 rewires TH17 cell metabolism via impeding PKM2 nuclear translocation. Cell Rep. 41, 111741 (2022).
Kaufmann, U. et al. Calcium signaling controls pathogenic TH17 cell-mediated inflammation by regulating mitochondrial function. Cell Metab. 29, 1104–1118.e6 (2019).
Wang, C. et al. CD5L/AIM regulates lipid biosynthesis and restrains TH17 cell pathogenicity. Cell 163, 1413–1427 (2015).
Chatterjee, S. et al. CD38–NAD+ axis regulates immunotherapeutic anti-tumor T cell response. Cell Metab. 27, 85–100.e8 (2018).
Bawden, E. G. et al. CD4+ T cell immunity against cutaneous melanoma encompasses multifaceted MHC II–dependent responses. Sci. Immunol. 9, eadi9517 (2024).
Mucida, D. et al. Transcriptional reprogramming of mature CD4+ helper T cells generates distinct MHC class II-restricted cytotoxic T lymphocytes. Nat. Immunol. 14, 281–289 (2013).
Fonseca, R. et al. Runx3 drives a CD8+ T cell tissue residency program that is absent in CD4+ T cells. Nat. Immunol. 23, 1236–1245 (2022).
Wang, Y. et al. The transcription factors T-bet and runx are required for the ontogeny of pathogenic interferon-γ-producing T helper 17 cells. Immunity 40, 355–366 (2014).
Śledzińska, A. et al. Regulatory T cells restrain interleukin-2- and blimp-1-dependent acquisition of cytotoxic function by CD4+ T cells. Immunity 52, 151–166.e6 (2020).
Serroukh, Y. et al. The transcription factors runx3 and ThPOK cross-regulate acquisition of cytotoxic function by human TH1 lymphocytes. eLife 7, e30496 (2018).
Ciucci, T. et al. The emergence and functional fitness of memory CD4+ T cells require the transcription factor Thpok. Immunity 50, 91–105.e4 (2019).
Gagliani, N. et al. TH17 cells transdifferentiate into regulatory T cells during resolution of inflammation. Nature 523, 221–225 (2015).
Berod, L. et al. De novo fatty acid synthesis controls the fate between regulatory T and T helper 17 cells. Nat. Med. 20, 1327–1333 (2014).
Shi, L. Z. et al. HIF1α-dependent glycolytic pathway orchestrates a metabolic checkpoint for the differentiation of TH17 and Treg cells. J. Exp. Med. 208, 1367–1376 (2011).
Shin, B. et al. Mitochondrial oxidative phosphorylation regulates the fate decision between pathogenic TH17 and regulatory T cells. Cell Rep. 30, 1898–1909.e4 (2020).
Guo, Y. et al. Metabolic reprogramming of terminally exhausted CD8+ T cells by IL-10 enhances anti-tumor immunity. Nat. Immunol. 22, 746–756 (2021).
Eil, R. et al. Ionic immune suppression within the tumour microenvironment limits T cell effector function. Nature 537, 539–543 (2016).
Larson, R. C. & Maus, M. V. Recent advances and discoveries in the mechanisms and functions of CAR T cells. Nat. Rev. Cancer 21, 145–161 (2021).
Fraietta, J. A. et al. Determinants of response and resistance to CD19 chimeric antigen receptor (CAR) T cell therapy of chronic lymphocytic leukemia. Nat. Med. 24, 563–571 (2018).
Wittling, M. C. et al. Distinct host preconditioning regimens differentially impact the antitumor potency of adoptively transferred TH17 cells. J. Immunother. Cancer 12, e008715 (2024).
Paulos, C. M. et al. The inducible costimulator (ICOS) is critical for the development of human TH17 cells. Sci. Transl. Med. 2, 55ra78 (2010).
Yu, C. et al. Human CD1c+ dendritic cells drive the differentiation of CD103+CD8+ mucosal effector T cells via the cytokine TGF-β. Immunity 38, 818–830 (2013).
Jung, I.-Y. et al. Tissue-resident memory CAR T cells with stem-like characteristics display enhanced efficacy against solid and liquid tumors. Cell Rep. Med. 4, 101053 (2023).
Wang, X. et al. Febrile temperature critically controls the differentiation and pathogenicity of T helper 17 cells. Immunity 52, 328–341.e5 (2020).
Xu, N. et al. STING agonist promotes CAR T cell trafficking and persistence in breast cancer. J. Exp. Med. 218, e20200844 (2021).
Ma, X. et al. Interleukin-23 engineering improves CAR T cell function in solid tumors. Nat. Biotechnol. 38, 448–459 (2020).
Benchetrit, F. et al. Interleukin-17 inhibits tumor cell growth by means of a T-cell–dependent mechanism. Blood 99, 2114–2121 (2002).