Credit: Westend61/ Getty Images
Credit: Westend61/ Getty Images
Researchers at Umeå University have identified how a toxin secreted by the cholera bacterium Vibrio cholerae can suppress colorectal cancer growth by altering the tumor microenvironment without harming healthy tissue. In mouse models, systemic administration of the purified cytotoxin MakA reduced tumor growth, increased cancer cell death, and reshaped immune cell activity within tumors, while showing no measurable toxicity. The findings, published in Cell Death & Disease, indicate that MakA acts both directly on tumor cells and indirectly by mobilizing innate immune responses, a finding that could provide a novel cancer treatment approach using bacterial products to target tumors.
“The substance not only kills cancer cells directly. It reshapes the tumor environment and helps the immune system to work against the tumor without damaging healthy tissue,” said lead author Sun Nyunt Wai, PhD, a professor of medical microbial pathogenesis at Umeå University.
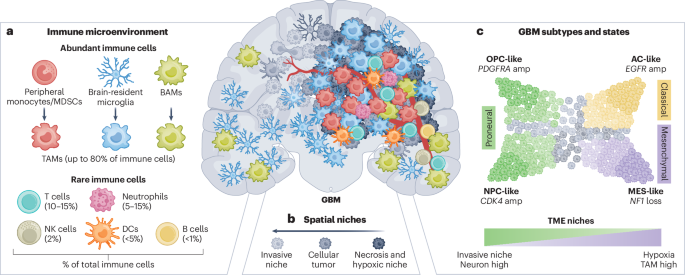
The study focused on colorectal cancer, which accounts for about 10% of all cancer diagnoses worldwide and is the second leading cause of cancer-related deaths. Existing treatments such as surgery, chemotherapy, and radiotherapy are effective for many patients but often come with significant side effects. The Umeå researchers sought to discovered whether MakA could offer a more targeted and less toxic treatment by influencing the tumor microenvironment, the complex network of cancer cells, immune cells, and signaling molecules that govern tumor progression.
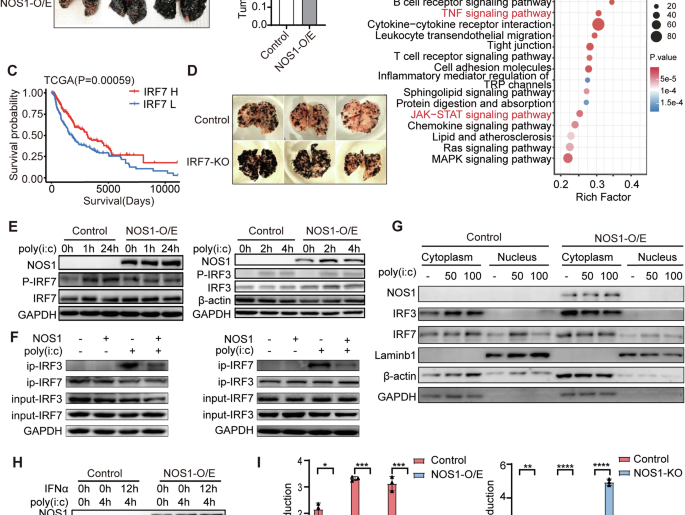
Previous studies from the Wai lab had identified MakA as a key virulence factor in V. cholerae, that produced cytotoxic effects in model organisms such as C. elegans and zebrafish. The toxin has been shown to bind to cell membranes and induce cancer cell death through mechanisms including apoptosis, altered autophagy, and reduced proliferation. Earlier experiments had also demonstrated that direct injection of MakA into tumors could inhibit colorectal tumor growth in mice. What remained unclear was whether the toxin could be given systemically, how safe that approach would be, and how MakA might influence immune cells within tumors.
To address these questions, the researchers used a mouse model of colorectal cancer and administered MakA systemically. They selected NOD/SCID mice, which lack functional T and B cells but retain innate immune components such as macrophages and neutrophils, allowing the researchers to focus on innate immune responses in the tumor microenvironment.
Analyses of the mice showed that MakA accumulated preferentially in tumor tissue and reduced cancer cell proliferation and increased apoptosis. It also altered the immune environment by increasing the presence of innate immune cells, particularly macrophages and neutrophils. A significant finding from this study was that the observed immune changes were localized to the tumor microenvironment and were not observed in organs such as the spleen, an indication that MakA did not trigger systemic immune activation.
While the effects of the immune activation remained localized, MakA did create a complex pattern of immune signaling. “The observed upregulation of pro-inflammatory mediators alongside anti-inflammatory cytokines suggests that MakA orchestrates a dual immune program amplifying inflammatory, potentially tumoricidal responses while simultaneously inducing regulatory mechanisms to prevent excessive tissue damage,” the researchers wrote.
The implications for clinical care and drug development are still in the early stages, but could be significant. “Although more research is needed, the results clearly show an interesting path for developing a new type of cancer treatment, which utilizes substances that bacteria create to both kill cancer cells and strengthen the body’s own defenses,” said senior author Saskia Erttmann, PhD, a professor at Umeå University.
Following on this promising study, the Umeå research will now study MakA in additional cancer, look to develop effective dosing strategies and develop a broad understanding the mechanisms at play that reprogrammed the immune response in the tumor microenvironment.