Key Takeaways
Vitamin D deficiency can lead to bone pain and fractures.People who spend a lot of time indoors or have dark skin are at risk for vitamin D deficiency.Vitamin D deficiency is often treated with vitamin D3 supplements.
Vitamin D is often referred to as the “sunshine vitamin” because it is produced by your body when your skin is exposed to the sun. Since vitamin D helps to keep your bones strong, a deficiency can lead to bone softening and subsequent bone pain and fractures.
1. You May Not Have Any Symptoms
Most people with vitamin D deficiency are asymptomatic. Only with a severe and prolonged deficiency do symptoms arise.
2. Bone and Muscle Symptoms in Severe Deficiency
The major role of vitamin D is to absorb calcium and phosphorus from the intestines in order to build and maintain bone mass. With vitamin D deficiency, this cannot occur adequately. With a severe deficiency, bone softening (a condition called osteomalacia in adults and rickets in children) may develop.
With osteomalacia and rickets, a person may experience throbbing bone discomfort and muscle weakness and pain. Osteomalacia also increases a person’s chances of developing bone fractures, falling, and experiencing walking problems.
3. Fatigue and Depression
Besides bone and muscle symptoms, fatigue and depression are also associated with vitamin D deficiency.
What Causes Vitamin D Deficiency?
Since you need sun exposure to make vitamin D, the most at-risk populations for vitamin D deficiency include anyone who spends a lot of time indoors (the elderly and the homebound, for example) and people with dark skin (as it produces less vitamin D from sunlight exposure).
Other populations at risk for vitamin D deficiency include:
Those who do not consume enough vitamin D-containing foods (e.g., canned tuna and fortified cow’s milk)
Those with diseases that affect the absorption of vitamin D in the gut (e.g., celiac disease and Crohn’s disease)
Those with diseases that affect the metabolism of vitamin D into its active form (e.g., chronic kidney disease or liver disease)
Those with obesity (extra fat tissue hides away vitamin D instead of releasing it into the bloodstream)
Those who take medications that enhance the breakdown of vitamin D (e.g., anti-seizure medications)
Interesting Associations
Besides its primary function in calcium metabolism, vitamin D may play a role in reducing inflammation and moderating immune function in the body. This may be why research has found links between vitamin D deficiency and various autoimmune diseases like multiple sclerosis, rheumatoid arthritis, and type 1 diabetes.
How Is Vitamin D Deficiency Diagnosed?
If you have one or more risk factors for vitamin D deficiency—for example, if you live with obesity, or if you have chronic kidney disease or a gut malabsorption syndrome—your healthcare provider should screen you for vitamin D deficiency.
Certain symptoms may also prompt your healthcare provider to test for vitamin D deficiency, such as an increased number of falls, especially if you are elderly.
However, screening for vitamin D deficiency in a person without symptoms is currently not recommended.
A simple blood test called 25-hydroxyvitamin D or 25(OH)D can be used to diagnose vitamin D deficiency.
While there is no definitive consensus about what a normal, healthy vitamin D level is, the Institute of Medicine (IOM) defines it as follows:
Normal: 25 (OH)D level greater than 20 ng/mLInsufficient: 25 (OH)D level between 12 to 20 ng/mLDeficient: 25 (OH)D level less than 12 ng/mLHigh enough to cause adverse effects: 25 (OH)D greater than 50 ng/mL
How Is Vitamin D Deficiency Treated?
The treatment of vitamin D deficiency depends on a number of factors, such as the severity of the deficiency and whether certain underlying health problems exist.
That said, in the vast majority of cases, vitamin D deficiency is treated with a supplement.
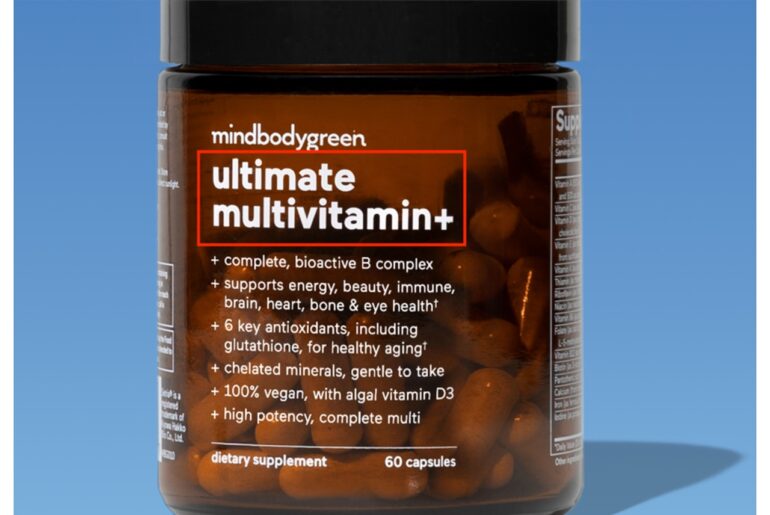
Supplements
There are two major forms of vitamin D: vitamin D2 (ergocalciferol) and vitamin D3 (cholecalciferol), the latter of which is used in most supplements.
To date, there is no standard regimen for treating vitamin D deficiency. A typical plan, though, may include taking 50,000 international units (IU) of vitamin D2 or D3 by mouth once a week for eight weeks, or 6,000 IU daily followed by a maintenance dose of 1,500 to 2,000 IU of vitamin D3 daily.
Keep in mind that higher doses will be needed to treat people with medical conditions that affect vitamin D absorption in the gut, and those taking medications that affect vitamin D metabolism.
Vitamin D Toxicity
Excess vitamin D may cause symptoms related to high calcium levels in the blood, such as muscle weakness, pain, heart arrhythmias, and kidney stones. This is why it is important to only take a vitamin D supplement as directed by your healthcare provider.
Food
Diet is an additional, although not robust, source of vitamin D, and therefore not usually recommended for treating a deficiency. That said, it can be useful for maintaining a healthy vitamin D level.
Foods that contain vitamin D include:
Fatty fish (e.g., salmon and swordfish)
Cod liver oil
Nuts
Cereals and dairy products fortified with vitamin D
Cheese
Eggs
Mushrooms
Beef liver
Sunlight
Sunlight is the third source of vitamin D. As with diet, it is not usually recommended as a treatment for vitamin D deficiency. This is because of the increased risk of skin cancer associated with sun exposure.
How Can You Prevent Deficiency?
While the amount of vitamin D that a person needs varies based on factors like skin color and sun exposure, general recommendations from the IOM state that individuals ages 1 to 70 should take a supplement containing 600 IU of vitamin D daily. After age 70, a person should take 800 IU of vitamin D daily.
These vitamin D preventive recommendations are for the general population—not for people with a diagnosed vitamin D deficiency. People who are deficient in vitamin D require therapeutic doses of vitamin D.
In addition to or in lieu of taking a supplement, your healthcare provider may recommend that you eat or drink foods that contain vitamin D and/or that you get some sunshine (but not too much).
What Does Vitamin D Have to Do With MS?
Verywell Health uses only high-quality sources, including peer-reviewed studies, to support the facts within our articles. Read our editorial process to learn more about how we fact-check and keep our content accurate, reliable, and trustworthy.
Nadeem S, Munim TF, Hussain HF, Hussain DF. Determinants of Vitamin D deficiency in asymptomatic healthy young medical students. Pak J Med Sci. 2018 Sep-Oct;34(5):1248-1252. doi:10.12669/pjms.345.15668
Institute of Medicine (US) Committee to Review Dietary Reference Intakes for Vitamin D and Calcium; Ross AC, Taylor CL, Yaktine AL, et al., editors. Dietary Reference Intakes for Calcium and Vitamin D. Washington (DC): National Academies Press (US).
Cleveland Clinic. Osteomalacia.
Roy S, Sherman A, Monari-Sparks MJ, Schweiker O, Hunter K. Correction of low Vitamin D improves fatigue: Effect of correction of low Vitamin D in fatigue study (EViDiF study). N Am J Med Sci. 2014 Aug;6(8):396-402. doi:10.4103/1947-2714.139291
Wong SK, Chin KY, Ima-Nirwana S. Vitamin D and depression: The evidence from an indirect clue to treatment strategy. Curr Drug Targets. 2018;19(8):888-97. doi:10.2174/1389450118666170913161030
Nair R, Maseeh A. Vitamin D: the “sunshine” vitamin. J Pharmacol Pharmacother. 2012;3(2):118-26. doi:10.4103/0976-500X.95506
National Institutes of Health. Office of Dietary Supplements. Vitamin D fact sheet for health professionals.
Cleveland Clinic. Vitamin D deficiency.
Harrison SR, Li D, Jeffery LE, Raza K, Hewison M. Vitamin D, autoimmune disease and rheumatoid arthritis. Calcif Tissue Int. 2020;106(1):58-75. doi:10.1007/s00223-019-00577-2
Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96(7):1911-1930. doi:10.1210/jc.2011-0385
US Preventive Services Task Force, Krist AH, Davidson KW, et al. Screening for vitamin D deficiency in adults: US Preventive Services Task Force Recommendation Statement. JAMA. 2021;325(14):1436. doi:10.1001/jama.2021.3069
Ross AC et al. The 2011 report on dietary reference intakes for calcium and vitamin D from the Institute of Medicine: what clinicians need to know. J Clin Endocrinol Metab. 2011 Jan;96(1):53-8. doi:10.1210/jc.2010-2704
Pilz S, Zittermann A, Trummer C, et al. Vitamin D testing and treatment: a narrative review of current evidence. Endocr Connect. 2019;8(2):R27-R43. doi:10.1530/EC-18-0432
Mark Stibich, PhD, FIDSA, is a behavior change expert with experience helping individuals make lasting lifestyle improvements.
Thanks for your feedback!
What is your feedback?
Helpful
Report an Error
Other