Clinical trials needed to test new combination of inhibitory drugs
NEW YORK, Feb. 11, 2026 /PRNewswire/ — A molecule that helps regulate gene activity has also been shown to drive skin cancer growth and tumors’ ability to evade attack by the body’s immune system, a new study shows.
 (PRNewsfoto/NYU Langone Health) (PRNewsfoto/NYU Langone Health)
(PRNewsfoto/NYU Langone Health) (PRNewsfoto/NYU Langone Health)
Led by researchers at NYU Langone Health and its Perlmutter Cancer Center, the study showed that a key protein — the transcription factor HOXD13 — is essential to the blood vessel growth needed to fuel melanoma tumor cells with oxygen and nutrients. Transcription factors control the rate at which genetic instructions encoded in DNA build the proteins that make up bodily structures and carry messages.
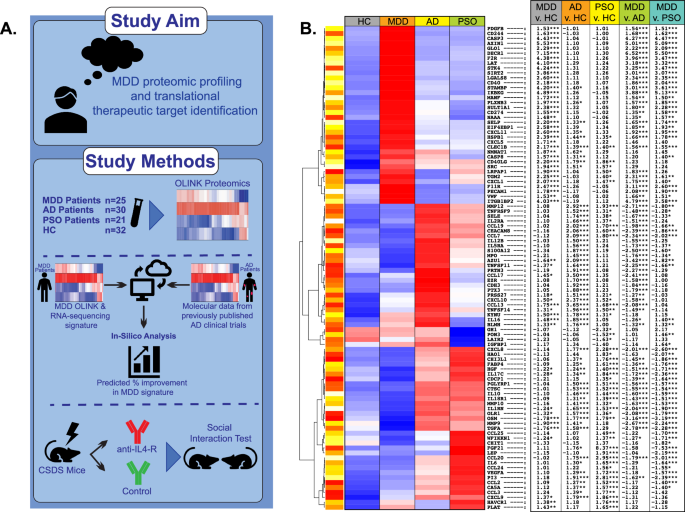
Publishing in the journal Cancer Discovery online Jan. 30, the researchers found that HOXD13 spurred activity in other signaling pathways that increase blood supply to tumors (angiogenesis), including those involving vascular endothelial growth factor (VEGF), semaphorin-3A (SEMA3A), and CD73. Experiments in which they suppressed HOXD13 activity led to tumor shrinkage.
The researchers also found that blood levels of cytotoxic T cells, which recognize cancer cells as abnormal and kill them, were lower in melanoma patients with high HOXD13 activity than in patients without the cancer or overactive HOXD13. The ability of such T cells to enter tumors was also reduced in melanoma patients with elevated HOXD13.
“Our study provides new evidence that transcription factor HOXD13 is a potent driver of melanoma growth and that it suppresses the T cell activity needed to fight the disease,” said study lead investigator Pietro Berico, PhD, a postdoctoral research fellow at the NYU Grossman School of Medicine and its Perlmutter Cancer Center.
Further, the study authors found that HOXD13 changes the environment around tumors to make it hostile to the immune function. It does this by boosting levels of another protein, CD73, which increases levels of adenosine, a substance that acts as a shield for the tumor by putting the brakes on T cells and preventing them from entering the tumor. When the researchers turned off HOXD13, they saw an increase in T cell infiltration into tumors.
“This data supports the combined targeting of angiogenesis and adenosine-receptor pathways as a promising new treatment approach for HOXD13-driven melanoma,” said study senior investigator Eva Hernando-Monge, PhD, a professor in the Department of Pathology at the NYU Grossman School of Medicine and a member of the Perlmutter Cancer Center.
Hernando-Monge says separate clinical trials are already underway evaluating the safety, dose tolerance, and efficacy of either VEGF-receptor and adenosine-receptor inhibitor medications for melanoma and other cancers. Some trials combined one of these inhibitors with another immunotherapy (drugs that harness the immune system to attack cancer.)
Story Continues
If these experiments prove successful, she says her team has plans for initiating clinical investigation on using a combination of VEGF and adenosine-receptor inhibitors to treat melanoma in those whose tumors show elevated HOXD13 levels.
Hernando-Monge also plans to investigate whether VEGF and adenosine pathways are potential targets for other cancers in which increased HOXD13 is present, including some glioblastomas, sarcomas, and osteosarcomas.
For the study, researchers analyzed tumors from over 200 melanoma patients from the U.S., Brazil, and Mexico, to see what pathways were elevated or suppressed. HOXD13 was among those that stood out. Further experiments in mice and human melanoma cell lines showed that HOXD13 also drove the other pathways involved in angiogenesis and immune evasion. Tests involving inhibition of HOXD13, VEGF, and adenosine then confirmed that HOXD13 was key to the cancer’s growth and survival.
Funding for this study was provided by National Institutes of Health grants P30CA016087, R01CA274100, P50CA225450, and U54CA263001, with additional support provided by the Melanoma Research Foundation, the Melanoma Research Alliance, United Kingdom Medical Research Council grant MR/S01473X/1, Brazilian National Council for Scientific and Technological Development (CNPQ) grants 442091/2023-0 and 309661/2023-4, and Wellcome Trust Career Development Award 227228/Z/23/Z.
In addition to Hernando-Monge and Berico, NYU Langone researchers involved in this study are co-investigators Amanda Flores Yanke, Fatemeh Vand Rajabpour, Catherine Do, Ines Delclaux, Tara Muijlwijk, Robert Stagnitta, Theodore Sakellaropoulos, Michelle Krogsgaard, Ata Moshiri, Iman Osman, Jane Skok, Amanda Lund, and Markus Schober.
Other researchers are study co-investigators Irving Wilmer and M. Estefania Vazquez-Cruz, and study principal investigator Carla Daniela Robles-Espinoza, at the National Autonomous University of Mexico in Juriquilla; and co-investigators Matheus Riberio and Annie Squiavinato, and study principal investigator Patricia Possik, at the Brazilian National Cancer Institute in Rio de Janeiro.
About NYU Langone Health
NYU Langone Health is a fully integrated health system that consistently achieves the best patient outcomes through a rigorous focus on quality that has resulted in some of the lowest mortality rates in the nation. Vizient Inc. has ranked NYU Langone No. 1 out of 118 comprehensive academic medical centers across the nation for four years in a row, and U.S. News & World Report recently ranked four of its clinical specialties No. 1 in the nation. NYU Langone offers a comprehensive range of medical services with one high standard of care across seven inpatient locations, its Perlmutter Cancer Center, and more than 320 outpatient locations in the New York area and Florida. The system also includes two tuition-free medical schools, in Manhattan and on Long Island, and a vast research enterprise.
DOI
10.1158/2159-8290.CD-24-1853
Media Contact:
David March
(212) 404-3528
David.March@nyulangone.org
Cision
View original content to download multimedia:https://www.prnewswire.com/news-releases/molecule-found-to-drive-skin-cancer-growth-and-evade-immune-detection-302680753.html